Introduction
Rhinosinusitis is a significant health problem which seems to
mirror the increasing frequency of allergic rhinitis and which
results in a large financial burden on society (1) . The last
decade has seen the development of a number of guidelines,
consensus documents and position papers on the epidemiology,
diagnosis and treatment of rhinosinusitis and nasal polyposis
(1-6). In 2005 the first European Position Paper on
Rhinosinusitis and Nasal Polyps (EP3 OS) was published (4, 7).
This first evidence based position paper was initiated by the
European Academy of Allergology and Clinical Immunology (EAACI)
to consider what was known about rhinosinusitis and nasal
polyps, to offer evidence based recommendations on diagnosis and
treatment, and to consider how we could make progress with
research in this area. The paper was endorsed by the European
Rhinologic Society. Such was the interest in the topic and the
increasing number of publications that by 2007 we felt it
necessary to update the document: EP3 OS2007 (1, 5). These new
publications included some important randomized controlled
trials and filled in some of the gaps in our knowledge, which
has significantly altered our approach. In particular it has
played an important role in the understanding of the management
of ARS and has helped to minimize unnecessary use of
radiological investigations, overuse of antibiotics, and improve
the under utilisation of nasal corticosteroids (8). EP3 OS2007
has had a considerable impact all over the world but as expected
with time, many people have requested that we revise it, as once
again a wealth of new data has become available in the
intervening period. Indeed one of its most important roles has
been in the identification of the gaps in the evidence and
stimulating colleagues to fill these with high quality studies.
The methodology for EPOS2012 has been the same as for the other
two productions. Leaders in the field were invited to critically
appraise the literature and write a report on a subject assigned
to them. All contributions were distributed before the meeting
in November when the group came together in Amsterdam and during
the 4 days of the meeting every report was discussed in detail.
In addition general discussions on important dilemmas and
controversies took place. Finally the management schemes were
revised significantly in the light of any new data which was
available. Finally we decided to remove the "3" out of EPOS2012
title (EPOS212 instead of EP3 OS2012) to make it more easy to
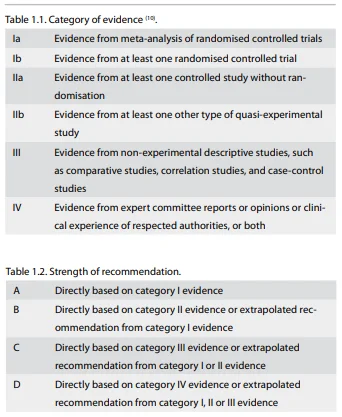
reproduce. Evidence based medicine is an important method of
preparing guidelines. In 1998 the Centre for Evidence Based
Medicine (CEBM) published its levels of evidence, which were
designed to help clinicians and decision makers to make the most
out of the available literature. Recently the levels of evidence
were revised in the light of new concepts and data (Table 1).
Moreover a number of other systems which grade the quality of
evidence and strength of recommendation have been proposed. The
most important of these is probably the GRADE initiative (9).
For the EPOS2012 we have chosen to collect the evidence using
the orginal CEBM format but we plan to update the EPOS2012
clinical recommendations subsequently, following the approach
suggested by the GRADE working group
This EPOS 2012 revision is intended to be a state-of-the art
review for the specialist as well as for the general
practitioner:
- to update their knowledge of rhinosinusitis and nasal poly-posis;
-
to provide an evidence based review of the diagnostic
methods;
-
to provide an evidence-based review of the available
treatments;
-
to propose a stepwise approach to the management of the
disease;
- to propose guidance for definitions and outcome measurements in research in different settings.