Acute Rhinosinusitis
- 3.5.3. Orbital complications of ARS
- 3.5.4. Endocranial complications
- 3.5.5. Cavernous sinus thrombosis
- 3.5.6. Bone complications
3.1. Epidemiology and predisposing factors of ARSSummary
ARS is a very common condition that is primarily managed in primary care. Prevalence rates vary from 6-15% depending on the study parameters, although studies specifying ARS report 6-12%, with a prevalence of recurrent ARS estimated at 0.035%. The primary cause of ARS are viruses with 0.5-2.0% of patients developing acute bacterial rhinosinusitis secondary to a viral infection. Prevalence of ARS varies with season (higher in the winter months) and climatic variations, and increasing with a damp environment and air pollution.
There appears to be overwhelming bodies of evidence to support the hypotheses that on-going allergic inflammation and cigarette smoke exposure predispose patients to ARS possibly via changes to ciliary motility and function. However, the role of laryngopharyngeal reflux in ARS is unclear. Chronic concomitant disease in children, poor mental health, and anatomical variations have been associated with an increased likelihood of ARS. Although ciliary function is altered in ARS, there is little evidence to support a role for ARS in primary cilia dyskinesia progression.
Further research is required to elucidate the underlying mechanisms by which on-going allergy and cigarette smoke exposure increases susceptibility to ARS is urgently needed. This review found that there is a paucity of studies characterising patients with ARS and concomitant diseases. Characterisation studies are required to identify possible co-existing or predisposing diseases beyond allergy, smoking, and possibly laryngopharyngeal reflux.
3.1.1. Epidemiology of ARS
ARS is highly prevalent, affecting 6-15% of the population
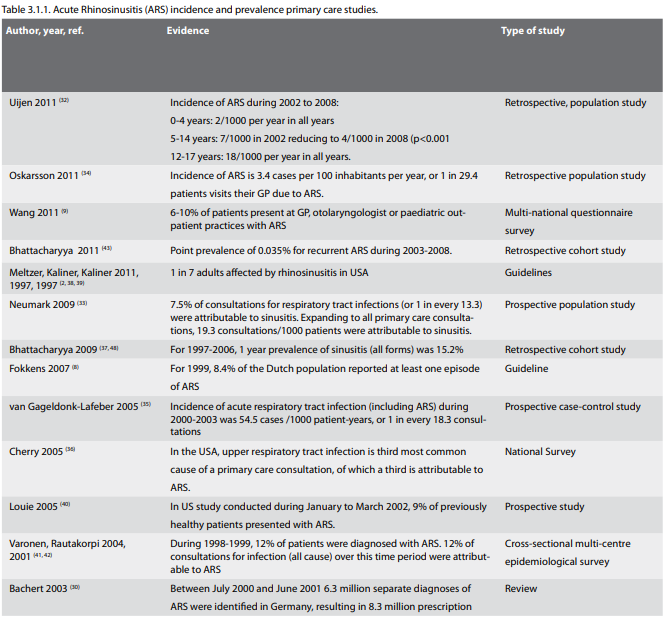
The incidence of acute sinusitis or rhinosinusitis (ARS) is very high, as previously described (8) and as summarised in Table 3.1.1. It has been estimated that adults suffer two to five episodes of viral ARS (or colds) per year and school children may suffer seven to ten colds per year (8, 30). Approximately 0.5-2% of viral upper respiratory tract infections are complicated by bacteria infection (8, 31). In a recent analysis of ENT problems in children using data from Dutch general practices participating in the Netherlands Information Network of General Practice from 2002 to 2008, Uijen et al. (32) reported stable incident rates of 18 cases of sinusitis per 1000 children aged 12-17 years per year and 2 cases per 1000 children in those aged 0-4 years. In children aged 5-11, Uijen et al. observed a decreasing incidence from 7 cases per 1000 children in 2002 down to 4/1000 in 2008 (p<0.001). In contrast, using the data for 240,447 consultations for a respiratory tract infection obtained from the EPR system Swedestar database, Neumark et al. (33) reported only a 2.5% decrease in consultations for sinusitis over the period from 1999 to 2005. In a small study, Oskarsson and Halldόrsson (34) reported an incidence of 3.4 cases per 100 inhabitants per year of acute sinusitis across a population derived from three health care centres in Iceland.
In Germany, from July 2000 to June 2001, 6.3 million separate diagnoses of ARS were identified resulting in 8.3 million prescriptions (30). In a three-year case-control study of the Dutch population, van Gageldonk-Lafeber estimated that annually, 900,000 individual patients consulted their primary care physician for acute respiratory tract infection (35). In the USA, upper respiratory tract infection is the third most common reason for a primary care provider consultation, with approximately a third of these attributed to ARS (36). Reported in 2009 and using data from the US National Health Interview Survey for years 1997 through to 2006, Bhattacharyya reported a 1-year disease prevalence of 15.2%, although the author discusses that this is likely to include both ARS and CRS. USA guidelines suggest that rhinosinusitis affects a reported 1 in 7 adults (37-39). Specifically focusing on ARS, an average of 8.4% of the Dutch population reported at least one episode of ARS per year in 1999 (8), while during January to March 2002, 9% (23 of 266 patients) of previously healthy patients presented with ARS at a Medical Centre Clinic in San Francisco, USA (40). In the Finnish MIKSTRA study conducted during 1998 and 1999, 12% (1601 of 13740) of patients were diagnosed with acute maxillary sinusitis (41). Using the same database, Rautakorpi (42) reported that 12% of consultations for infection were attributed to sinusitis. In Asia, an estimated 6-10% of patients seen at GP, otolaryngologist, and 3. Acute Rhinosinusitis 10 European Position Paper on Rhinosinusitis and Nasal Polyps 2012 paediatrician outpatient practices present with ARS (9). Recurrent ARS may be considered distinct from ARS and CRS. Using data from a medical claims database for 13.1 million patients from 2003 to 2008, the point prevalence of recurrent ARS has been reported to be 0.035%, and considerably lower than that of ARS (43). Whether recurrent ARS should be considered a form of acute or CRS requires further discussion.
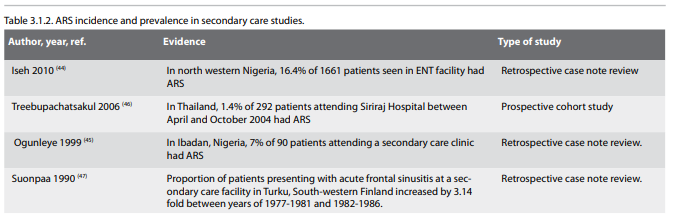
A number of studies have described patients attending secondary
care facilities for acute rhinosinusitis as summarised in Table
3.1.2. In North-western Nigeria, 195 of 1661 patients seen in a
secondary care ENT facility presented with rhinosinusitis, of
which 16.4% had ARS (44). The proportion of patients with acute
rhinitis was considerably higher than had been previously
reported by Ogunleye et al. in 1999 (45). In a retrospective
review of 90 patients attending a secondary care clinic in
Ibadan, Nigeria, they reported that only 7% of the 90 patients
were identified as having ARS (45). A prevalence of ARS of 1.4%
was reported in a 292 patient study of upper respiratory tract
infections presenting at Siriraj Hospital, Thailand, between
April and October 2004 (46). This low prevalence may be due to
the majority of patients with ARS presenting to their primary
care provider rather than hospital. An increasing prevalence of
sinusitis has been reported in Turku in south-western Finland,
in which a 3.14 fold increase in the number of patients
presenting with acute frontal sinusitis at a secondary care
facility was observed between 1977-81 (134 patients) and
1982-1986 (421 patients) (47). While this may be as a result of
increasing diagnosis and willingness to refer to secondary care,
Suonpaa and Antila (47) suggest that increasing air pollution in
the city area of Turku may be partly responsible.
3.1.2. Factors associated with ARS
Identifying factors predictive of ARS and/or acute respiratory tract infections could aid resource availability.
3.1.2.1. Environmental Exposures
Using a matched case control study design conducted in a Dutch population over the period of 2000 to 2003, van Gageldonk-Lafeber et al. (50) reported that exposure to an individual(s) with respiratory complaints, inside or outside of the immediate household was an independent risk factor for attending their GP with an acute respiratory tract infection (adjusted OR = 1.9 and adjusted OR = 3.7, respectively). In contrast, patients with children in secondary education, who had dampness or mould at home, or had exposure to passive smoking were less likely to visit their GP compared to those without children, mould or dampness or passive smoking exposure respectively. Increased levels of dampness, but not mould, in the home has been associated with sinusitis (51).
Seasonal trends in occurrences of ARS have been reported. In a study of respiratory tract infections, Neumark et al. (33) reported seasonal variable in the incidence rate of sinusitis from 1999 through to 2005, with increased incidence in the first quarter of each year. For acute respiratory illnesses in 2000 to 2003, van Gageldonk-Lafeber et al. (35) reported similar seasonal trends to those of Neumark. Compared to July to September, van Gageldonk-Lafeber et al reported that the relative risk of acquiring an acute respiratory illness was 2.9 (95% CI: 2.8- 3.0) in January to March, 1.8 (95% CI: 1.7-1.9) in October to December and 1.4 (95% CI: 1.3-1.5) in April to June. In an audit of complications of ARS, Babar-Craig et al. (52) reported that 69% of patients were admitted during the winter months of November to April. Similar patterns have been reported in acute exacerbations of CRS (53) and upper respiratory tract infections (54). Climate variations have been reported to induce facial pain similar to ARS. Chinook, or föhn, is a weather event in which a rapidly moving warm, high-pressurised wind enters into a specific location. The pressure changes that occur during the Chinook induce facial pain similar to that experienced in sinusitis pain. Rudmik et al. (55) report that compared to controls, the presence of concha bullosa and spheno ethmoidal cell (Onodi cell; p=0.004), and larger maxillary sinus size (right, p=0.015; left, p=0.002) are all associated with complaints of Chinook headache.
However, as the Lund-Mackay score was higher in the control group, the authors conclude that CRS is unlikely to be associated with the Chinook induced facial pain. Exposure to air pollution (47, 48, 56), irritants used in the preparation of pharmaceutical products (57), during photocopying (58) and forest fire smoke (59) have all been associated with an increase in the prevalence of symptoms of ARS.
3.1.2. Factors associated with ARS
Identifying factors predictive of ARS and/or acute respiratory tract infections could aid resource availability.
3.1.2.1. Environmental Exposures
Using a matched case control study design conducted in a Dutch population over the period of 2000 to 2003, van Gageldonk-Lafeber et al. (50) reported that exposure to an individual(s) with respiratory complaints, inside or outside of the immediate household was an independent risk factor for attending their GP with an acute respiratory tract infection (adjusted OR = 1.9 and adjusted OR = 3.7, respectively). In contrast, patients with children in secondary education, who had dampness or mould at home, or had exposure to passive smoking were less likely to visit their GP compared to those without children, mould or dampness or passive smoking exposure respectively. Increased levels of dampness, but not mould, in the home has been associated with sinusitis (51).
Seasonal trends in occurrences of ARS have been reported. In a study of respiratory tract infections, Neumark et al. (33) reported seasonal variable in the incidence rate of sinusitis from 1999 through to 2005, with increased incidence in the first quarter of each year. For acute respiratory illnesses in 2000 to 2003, van Gageldonk-Lafeber et al. (35) reported similar seasonal trends to those of Neumark. Compared to July to September, van Gageldonk-Lafeber et al reported that the relative risk of acquiring an acute respiratory illness was 2.9 (95% CI: 2.8- 3.0) in January to March, 1.8 (95% CI: 1.7-1.9) in October to December and 1.4 (95% CI: 1.3-1.5) in April to June. In an audit of complications of ARS, Babar-Craig et al. (52) reported that 69% of patients were admitted during the winter months of November to April. Similar patterns have been reported in acute exacerbations of CRS (53) and upper respiratory tract infections (54). Climate variations have been reported to induce facial pain similar to ARS. Chinook, or föhn, is a weather event in which a rapidly moving warm, high-pressurised wind enters into a specific location. The pressure changes that occur during the Chinook induce facial pain similar to that experienced in sinusitis pain. Rudmik et al. (55) report that compared to controls, the presence of concha bullosa and spheno ethmoidal cell (Onodi cell; p=0.004), and larger maxillary sinus size (right, p=0.015; left, p=0.002) are all associated with complaints of Chinook headache.
However, as the Lund-Mackay score was higher in the control group, the authors conclude that CRS is unlikely to be associated with the Chinook induced facial pain. Exposure to air pollution (47, 48, 56), irritants used in the preparation of pharmaceutical products (57), during photocopying (58) and forest fire smoke (59) have all been associated with an increase in the prevalence of symptoms of ARS.
3.1.2.2. Anatomical factors
Anatomical factors including Haller cells, concha bullosa, septal deviation, choanal atresia, nasal polyps and hypoplasia of sinuses have all been associated with ARS. In a sinus computed tomography study of recurrent ARS versus non rhinosinusitis controls, Alkire and Bhattacharyya (60) reported significantly higher Lund score (2.25 versus 1.27; p<0.001), higher frequency of Haller cells on radiograph (39.9% versus 11.9%; p=0.006) and smaller mean infundibular widths (0.591 mm versus 0.823 mm; p<0.001) compared to controls. They also reported a higher frequency of concha bullosa (41.7% versus 28.6%) and impinging septal spurs (27.8% versus 19.0%) than controls, although neither reached statistically significance. Suonpaa and Antila (47) reported an increase in the occurrence of nasal polyps in their study of ARS between 1977-1981 and 1982-1986.
In patients with recurrent ARS, anatomical variations including Haller cells and septal deviation, nasal polyps, septal deviation, and choanal obstruction by benign adenoid tissue, or odontogenic sources of infections should be considered.
Odontogenic infections, or infections arising from dental sources, causing acute maxillary sinusitis have been reported in the literature. Bomeli et al. (61) reported that oroantral fistula and periodontal disease plus either a projecting tooth root or periapical abscess were significantly identified as sources of acute maxillary sinusitis. Furthermore they demonstrated that the greater the extent of fluid opacification and mucosal thickening, the greater the likelihood of an identifiable dental infective source. In a computed tomography (CT) radiological study of the maxillary sinus in elderly dentate and edentulous patients, Mathew et al. (62) reported an increased prevalence of mucosal thickenings (74.3 versus 25.6; p<0.05) and mucous cysts (2.1% versus 0) in dentate patients compared to edentate controls.
In a study of 76 children presenting with ARS, Eyigör and Basak (63) reported that 16 (21.1%) had septal deviation, and 25 (32.9%) had choanal obstruction by benign adenoid tissue.
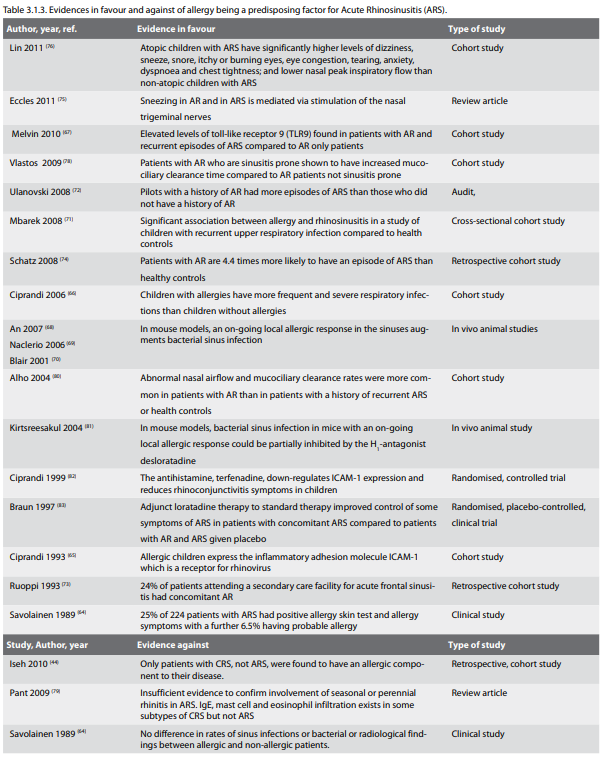
3.1.2.3. Allergy
The role of allergy in ARS is the subject of much debate with literature both supporting and disputing a role for allergy in predisposing for ARS, as summarised in Table 3.1.3. In 1989, Savolainen (64) reported that 25% of 224 patients with acute maxillary sinusitis had allergy, as verified by allergy questionnaire, skin testing and nasal smears, with a further 6.5% of patients having probable allergy. However, upon comparison of those with and without allergy, no differences were found in the number of previous episodes of ARS, or bacteriological and radiological findings suggesting that the presence of allergy maybe incidental. In 1993, Ciprandi et al. (65) demonstrated that expression of the inflammatory adhesion molecule, ICAM-1, is elevated in patients with AR exposed to allergen challenge. As ICAM-1 has been shown to be a receptor molecule for rhinovirus, the authors hypothesise that increased expression of ICAM-1 maybe responsible for increased susceptibility to respiratory infections in patients with allergy (66). More recently Melvin et al. (67) demonstrated that patients with AR and recurrent episodes of ARS had elevated expression of the tolllike receptor 9 (TLR9) in the sinonasal epithelium compared to patients with only AR, suggesting that TLR9 may be upregulated in response to repeated microbial insults. The authors theorise that impairment of innate immune gene expression may predispose some patients with AR to subsequent development of recurrent ARS. In a mouse model of AR, An et al. (68) reported that mice with significant mucosal oedema and dilate venules due to ovalbumin induced AR (and sensitisation) had significantly higher polymorphonuclear neutrophils (PMN) and eosinophils following exposure to S. pneumoniae than mice with induced AR exposed to saline. Furthermore, mice without induced AR, but sensitised to ovalbumin and exposed to S. pneumoniae, had significantly lower PMN but comparable eosinophils and IL-5 levels to those sensitised and with AR, suggesting that an on-going allergic response, but not sensitisation, increases the likelihood of S pneumoniae sinus infection. Naclerio et al. (69) and Blair et al. (70) reported comparable results.
Clinically, ARS has been associated with atopy and AR. In a cross-sectional cohort study of 100 children presenting with recurrent upper respiratory tract infections compared to 164 healthy controls, Mbarek et al. (71) reported a significant association between allergy and rhinosinusitis (p=0.001), as well as recurrent upper respiratory tract infections (p=0.01), rhinopharyngitis (p=0.02) and acute otitis media (p=0.01). In a comparative case – control study of Israeli air force pilots, Ulanovski (72) reported that 33% of pilots with a history of AR and 21% of the control group had one or more episodes of ARS (p=0.09). Restricting to those pilots aged <26 years of age, the resultant findings were 57% and 29% (p<0.001), respectively. Stratification of pilots with a history of AR by pilot type showed that 54% of transport pilots, 34% of fighter pilot and 13% of helicopter pilots has also had one or more episodes of ARS, compared to the 28%, 15% and 15% of pilots in the control group. The authors theorise that the lower prevalence of ARS in the fighter pilot group as compared to the transport pilots with a history of AR may be attributable to vasoconstriction due to psychological and physiological stress exhibited during flight missions. In a retrospective analysis of patients presenting with frontal ARS between 1981 and 1990 at a secondary care facility in Kuopio, Ruoppi et al. (73) reported that 22 of the 91 (24%) patients identified had concomitant AR. Schatz et al. (74) reported that the odds of developing an episode of ARS was 4.4 times higher in patients with rhinitis than in healthy controls. Symptomatically, Eccles considered the association of sneezing in AR and also in ARS to indicate a potential link between the two conditions via stimulation of the nasal trigeminal nerves (75). Indeed, symptom scores for 'sneeze' were higher in children with atopy and ARS than those with rhinosinusitis alone (76), while ARS has been shown to produce bilaterial large myelinated fibre hypersensitivity of the trigeminal nerves compared to healthy controls (77).
Evidence also suggests that AR is associated with impaired mucociliary clearance (78). In a prospective study of 125 patients with AR, using the saccharine test, Vlastos et al. (78) reported that 23 patients with AR who were sinusitis prone had a significantly greater mucociliary clearance time as compared to 102 control patients with AR but not sinusitis prone (12 and 15 minutes, respectively; p=0.02). Further research is required to explore this predisposition for rhinosinusitis in AR. In 2009, Pant et al. (79) undertook a review of allergy in rhinosinusitis. In contrast to the above literature, Pant et al concluded that insufficient evidence exists to confirm seasonal or perennial AR as a significant predisposing factor for ARS. However, they do confirm that an association between IgE, mast cell, and eosinophil infiltration exists in some subtypes of CRS, but not ARS. In contrast to this review, Lin and cols. recently reported that children with atopy were more likely to develop ARS (76). They reported that atopic children with ARS reported significantly higher symptoms (including dizziness, sneeze, snore, itchy or burning eyes, eye congestion and tearing) as well as significantly higher levels of anxiety, dyspnoea, chest tightness, and lower nasal peak inspiratory flow than non-atopic children with ARS. Alho (80) reported that during viral ARS (or cold), a greater proportion of patients with concomitant AR had abnormal nasal airflow, mucociliary clearance and higher ipsilaterial paranasal sinus CT scores than patients with a history of recurrent ARS or healthy controls.
Anatomical factors including Haller cells, concha bullosa, septal deviation, choanal atresia, nasal polyps and hypoplasia of sinuses have all been associated with ARS. In a sinus computed tomography study of recurrent ARS versus non rhinosinusitis controls, Alkire and Bhattacharyya (60) reported significantly higher Lund score (2.25 versus 1.27; p<0.001), higher frequency of Haller cells on radiograph (39.9% versus 11.9%; p=0.006) and smaller mean infundibular widths (0.591 mm versus 0.823 mm; p<0.001) compared to controls. They also reported a higher frequency of concha bullosa (41.7% versus 28.6%) and impinging septal spurs (27.8% versus 19.0%) than controls, although neither reached statistically significance. Suonpaa and Antila (47) reported an increase in the occurrence of nasal polyps in their study of ARS between 1977-1981 and 1982-1986.
In patients with recurrent ARS, anatomical variations including Haller cells and septal deviation, nasal polyps, septal deviation, and choanal obstruction by benign adenoid tissue, or odontogenic sources of infections should be considered.
Odontogenic infections, or infections arising from dental sources, causing acute maxillary sinusitis have been reported in the literature. Bomeli et al. (61) reported that oroantral fistula and periodontal disease plus either a projecting tooth root or periapical abscess were significantly identified as sources of acute maxillary sinusitis. Furthermore they demonstrated that the greater the extent of fluid opacification and mucosal thickening, the greater the likelihood of an identifiable dental infective source. In a computed tomography (CT) radiological study of the maxillary sinus in elderly dentate and edentulous patients, Mathew et al. (62) reported an increased prevalence of mucosal thickenings (74.3 versus 25.6; p<0.05) and mucous cysts (2.1% versus 0) in dentate patients compared to edentate controls.
In a study of 76 children presenting with ARS, Eyigör and Basak (63) reported that 16 (21.1%) had septal deviation, and 25 (32.9%) had choanal obstruction by benign adenoid tissue.
3.1.2.3. Allergy
The role of allergy in ARS is the subject of much debate with literature both supporting and disputing a role for allergy in predisposing for ARS, as summarised in Table 3.1.3. In 1989, Savolainen (64) reported that 25% of 224 patients with acute maxillary sinusitis had allergy, as verified by allergy questionnaire, skin testing and nasal smears, with a further 6.5% of patients having probable allergy. However, upon comparison of those with and without allergy, no differences were found in the number of previous episodes of ARS, or bacteriological and radiological findings suggesting that the presence of allergy maybe incidental. In 1993, Ciprandi et al. (65) demonstrated that expression of the inflammatory adhesion molecule, ICAM-1, is elevated in patients with AR exposed to allergen challenge. As ICAM-1 has been shown to be a receptor molecule for rhinovirus, the authors hypothesise that increased expression of ICAM-1 maybe responsible for increased susceptibility to respiratory infections in patients with allergy (66). More recently Melvin et al. (67) demonstrated that patients with AR and recurrent episodes of ARS had elevated expression of the tolllike receptor 9 (TLR9) in the sinonasal epithelium compared to patients with only AR, suggesting that TLR9 may be upregulated in response to repeated microbial insults. The authors theorise that impairment of innate immune gene expression may predispose some patients with AR to subsequent development of recurrent ARS. In a mouse model of AR, An et al. (68) reported that mice with significant mucosal oedema and dilate venules due to ovalbumin induced AR (and sensitisation) had significantly higher polymorphonuclear neutrophils (PMN) and eosinophils following exposure to S. pneumoniae than mice with induced AR exposed to saline. Furthermore, mice without induced AR, but sensitised to ovalbumin and exposed to S. pneumoniae, had significantly lower PMN but comparable eosinophils and IL-5 levels to those sensitised and with AR, suggesting that an on-going allergic response, but not sensitisation, increases the likelihood of S pneumoniae sinus infection. Naclerio et al. (69) and Blair et al. (70) reported comparable results.
Clinically, ARS has been associated with atopy and AR. In a cross-sectional cohort study of 100 children presenting with recurrent upper respiratory tract infections compared to 164 healthy controls, Mbarek et al. (71) reported a significant association between allergy and rhinosinusitis (p=0.001), as well as recurrent upper respiratory tract infections (p=0.01), rhinopharyngitis (p=0.02) and acute otitis media (p=0.01). In a comparative case – control study of Israeli air force pilots, Ulanovski (72) reported that 33% of pilots with a history of AR and 21% of the control group had one or more episodes of ARS (p=0.09). Restricting to those pilots aged <26 years of age, the resultant findings were 57% and 29% (p<0.001), respectively. Stratification of pilots with a history of AR by pilot type showed that 54% of transport pilots, 34% of fighter pilot and 13% of helicopter pilots has also had one or more episodes of ARS, compared to the 28%, 15% and 15% of pilots in the control group. The authors theorise that the lower prevalence of ARS in the fighter pilot group as compared to the transport pilots with a history of AR may be attributable to vasoconstriction due to psychological and physiological stress exhibited during flight missions. In a retrospective analysis of patients presenting with frontal ARS between 1981 and 1990 at a secondary care facility in Kuopio, Ruoppi et al. (73) reported that 22 of the 91 (24%) patients identified had concomitant AR. Schatz et al. (74) reported that the odds of developing an episode of ARS was 4.4 times higher in patients with rhinitis than in healthy controls. Symptomatically, Eccles considered the association of sneezing in AR and also in ARS to indicate a potential link between the two conditions via stimulation of the nasal trigeminal nerves (75). Indeed, symptom scores for 'sneeze' were higher in children with atopy and ARS than those with rhinosinusitis alone (76), while ARS has been shown to produce bilaterial large myelinated fibre hypersensitivity of the trigeminal nerves compared to healthy controls (77).
Evidence also suggests that AR is associated with impaired mucociliary clearance (78). In a prospective study of 125 patients with AR, using the saccharine test, Vlastos et al. (78) reported that 23 patients with AR who were sinusitis prone had a significantly greater mucociliary clearance time as compared to 102 control patients with AR but not sinusitis prone (12 and 15 minutes, respectively; p=0.02). Further research is required to explore this predisposition for rhinosinusitis in AR. In 2009, Pant et al. (79) undertook a review of allergy in rhinosinusitis. In contrast to the above literature, Pant et al concluded that insufficient evidence exists to confirm seasonal or perennial AR as a significant predisposing factor for ARS. However, they do confirm that an association between IgE, mast cell, and eosinophil infiltration exists in some subtypes of CRS, but not ARS. In contrast to this review, Lin and cols. recently reported that children with atopy were more likely to develop ARS (76). They reported that atopic children with ARS reported significantly higher symptoms (including dizziness, sneeze, snore, itchy or burning eyes, eye congestion and tearing) as well as significantly higher levels of anxiety, dyspnoea, chest tightness, and lower nasal peak inspiratory flow than non-atopic children with ARS. Alho (80) reported that during viral ARS (or cold), a greater proportion of patients with concomitant AR had abnormal nasal airflow, mucociliary clearance and higher ipsilaterial paranasal sinus CT scores than patients with a history of recurrent ARS or healthy controls.
3.1.2.4. Ciliary impairment
Ciliary impairment has been demonstrated to be a feature of both viral and bacterial rhinosinusitis (8). This includes both the loss of cilia and ciliated cells as well as a disruption of normal mucociliary flow. Smoking and allergy have been implicated in the disruption of cilia function. Indeed impaired mucociliary clearance in AR patients predisposes patients to ARS (78).
Ciliary function is diminished during viral and bacterial rhinosinusitis. Exposure to cigarette smoke and allergic inflammation has also been shown to impair ciliary function, although research is required to understand these processes further.
Ciliary impairment has also been associated with cigarette smoking. In vitro studies have demonstrated that cigarette smoke condensate and cigarette smoke extract impairs ciliogenesis in a dose-dependent manner (84). Clinical studies have also reported that exposure to passive smoking increases the levels of matrix metalloproteinase 9 (MMP-9), a gelatinase associated with tissue modelling is significantly increased in nasal secretions of children (85) exposed to passive smoking. As increased production of MMP-9 has been found in the acute allergic response in the nose and lungs, the implications for the involvement of MMP-9, ciliary function, allergic response, and smoking in ARS needs further exploration.
3.1.2.5. Primary Cilia Dyskinesia
Primary cilia dyskinesia (PCD) is a rare autosomal recessive disorder in which cilia are either immotile, or beat in such a pattern that there is failure to transport the airway mucous. PCD is associated with chronic upper airway symptoms including nasal discharge (episodic facial pain and anosmia) and bronchiectasis (86), with neonates presenting with continuous rhinorrhoea from the first day of life (87-89). Limited information is available on the prevalence of PCD. In a Norwegian study conducted in 1947 and 1949, prevalence of PCD was estimated at 1:40,000 (90). However, this radiological study was likely to be an underestimate due to limitations of standard chest radiographs in detecting bronchiectasis and that bronchiectasis may not have developed in the younger study patients. Using data from 1976 – 1990, the prevalence of PCD in Sweden has been estimated to range from 1:22,000 to 1:10,000 (91), the difference in prevalence due to the likely under-diagnosis of the condition. The highest prevalence, 1:4,100, was reported in a study of the impact of the Hiroshima and Nagasaki delayed atomic bombs (92). The frequency of episodes of ARS in these patients groups is not reported
In a study of 38 bronchiectasis patients, PCD was reported to be responsible for 13% of cases, and was more common in North African patients than European (93). Barbato et al. (94), for the European Respiratory Society Task Force on PCD, report that recurrent ARS in PCD patients is rare, although episodes should be treated with 'adequate and prolonged antibiotic(s)' (95-97). In agreement with the ERS Task Force, Bush et al. report that upper (and lower) airway infections should be treated aggressively, and that lung disease is usually stabilised once treatment is initiated. Although evidence exists to suggest that treating ARS will prevent recurrence or chronicity (49), whether this can applied to the PCD population is unknown. In the absence of lower airway infection, the impact of acute or recurrent ARS on the progression of PCD related bronchiectatic lung disease is unknown.
3.1.2.6. Smoking
Limited research exists on the impact of smoking on ARS. Using data from the 1970 National Health Interview Survey, and after excluding families with children with chronic respiratory illness, Bonham and Wilson (98) reported that children from households with one or more adult cigarette smokers had significantly more restricted activity and bed-disability days than did children from families with non-smoking adults. This difference was found to be due to children from families with active smokers having more episodes of acute respiratory illness (including ARS). Comparable significant results were found when families in which 45 cigarettes or more were consumed per day were compared to families with non-smoking adults. The authors concluded that higher cigarette consumption was associated with increased predisposition for acute respiratory illness. In a paediatric characterisation study of 76 patients with acute rhinosinusitis aged 4-18 years, Eyigör and Başak (63) reported that 51.3% (39 patients) were exposed to second hand smoke and 2.6% (2 patients) were active smokers. Based on their population, the authors concluded that exposure to primary or second hand smoke were predisposing factors for ARS. In a study characterising the respiratory symptoms of adult postal workers in Zagreb, Croatia, the prevalence of sinusitis in 15 Supplement 23 active smokers was 53.1% compared to 26.4% in non-smokers, although no information was available on whether the sinusitis was recurrent acute or chronic in nature (99).
Active smokers with on-going allergic inflammation have an increased susceptibility to ARS compared to non-smokers with on-going allergic inflammation, suggesting that exposure to cigarette smoke and allergic inflammation is mediated via different and possibly synergistic mechanisms. Research to elucidate these mechanisms is needed.
The impact of second-hand tobacco smoke on symptoms of rhinosinusitis has also been evaluated in patients with AR (100). This study reported that patients with AR exposed to second hand smoke had more symptoms consistent with rhinosinusitis including facial pain and facial congestion or fullness, and a greater proportion had received medication for rhinosinusitis including antibiotics for respiratory problems in the previous 12 weeks compared to disease specific controls. Although the authors did not evaluate the occurrences of ARS, the greater proportion of patients requiring antibiotics for respiratory problems would suggest that patients exposed to second-hand tobacco smoke may have had more episodes of ARS or recurrent ARS, although the authors do not delineate between antibiotics for upper or lower airway respiratory problems. Active and passive smoking has been shown to alter the normal bacterial flora present in the nasopharyngeal spaces, resulting in the colonisation of more potential pathogens than found in non-smokers (101). Following smoking cessation, the microbial population has been shown to revert back to that found in nonsmokers (102). The impact of smoking cessation programmes on the incidence and prevalence of ARS is unknown.
In vitro and in vivo studies have recently shown to increased MMP-9 production in children exposed to passive smokers (85) and increased complement activation in human respiratory epithelial cells and mice exposed to cigarette smoke extract (103). Whether increased MMP-9 production or complement activation due to exposure to cigarette smoke predisposes to ARS is unknown and requires further investigation.
3.1.2.7. Laryngopharyngeal reflux
Little is known about the association of ARS and laryngopharyngeal reflux. As reviewed by Pacheco-Galván et al. (104), epidemiological studies conducted between 1997 and 2006 have shown significant associations between GERD and sinusitis. However, in a recent systematic review, Flook and Kumar showed only a poor association between acid reflux, nasal symptoms, and ARS (105).
Ciliary impairment has been demonstrated to be a feature of both viral and bacterial rhinosinusitis (8). This includes both the loss of cilia and ciliated cells as well as a disruption of normal mucociliary flow. Smoking and allergy have been implicated in the disruption of cilia function. Indeed impaired mucociliary clearance in AR patients predisposes patients to ARS (78).
Ciliary function is diminished during viral and bacterial rhinosinusitis. Exposure to cigarette smoke and allergic inflammation has also been shown to impair ciliary function, although research is required to understand these processes further.
Ciliary impairment has also been associated with cigarette smoking. In vitro studies have demonstrated that cigarette smoke condensate and cigarette smoke extract impairs ciliogenesis in a dose-dependent manner (84). Clinical studies have also reported that exposure to passive smoking increases the levels of matrix metalloproteinase 9 (MMP-9), a gelatinase associated with tissue modelling is significantly increased in nasal secretions of children (85) exposed to passive smoking. As increased production of MMP-9 has been found in the acute allergic response in the nose and lungs, the implications for the involvement of MMP-9, ciliary function, allergic response, and smoking in ARS needs further exploration.
3.1.2.5. Primary Cilia Dyskinesia
Primary cilia dyskinesia (PCD) is a rare autosomal recessive disorder in which cilia are either immotile, or beat in such a pattern that there is failure to transport the airway mucous. PCD is associated with chronic upper airway symptoms including nasal discharge (episodic facial pain and anosmia) and bronchiectasis (86), with neonates presenting with continuous rhinorrhoea from the first day of life (87-89). Limited information is available on the prevalence of PCD. In a Norwegian study conducted in 1947 and 1949, prevalence of PCD was estimated at 1:40,000 (90). However, this radiological study was likely to be an underestimate due to limitations of standard chest radiographs in detecting bronchiectasis and that bronchiectasis may not have developed in the younger study patients. Using data from 1976 – 1990, the prevalence of PCD in Sweden has been estimated to range from 1:22,000 to 1:10,000 (91), the difference in prevalence due to the likely under-diagnosis of the condition. The highest prevalence, 1:4,100, was reported in a study of the impact of the Hiroshima and Nagasaki delayed atomic bombs (92). The frequency of episodes of ARS in these patients groups is not reported
In a study of 38 bronchiectasis patients, PCD was reported to be responsible for 13% of cases, and was more common in North African patients than European (93). Barbato et al. (94), for the European Respiratory Society Task Force on PCD, report that recurrent ARS in PCD patients is rare, although episodes should be treated with 'adequate and prolonged antibiotic(s)' (95-97). In agreement with the ERS Task Force, Bush et al. report that upper (and lower) airway infections should be treated aggressively, and that lung disease is usually stabilised once treatment is initiated. Although evidence exists to suggest that treating ARS will prevent recurrence or chronicity (49), whether this can applied to the PCD population is unknown. In the absence of lower airway infection, the impact of acute or recurrent ARS on the progression of PCD related bronchiectatic lung disease is unknown.
3.1.2.6. Smoking
Limited research exists on the impact of smoking on ARS. Using data from the 1970 National Health Interview Survey, and after excluding families with children with chronic respiratory illness, Bonham and Wilson (98) reported that children from households with one or more adult cigarette smokers had significantly more restricted activity and bed-disability days than did children from families with non-smoking adults. This difference was found to be due to children from families with active smokers having more episodes of acute respiratory illness (including ARS). Comparable significant results were found when families in which 45 cigarettes or more were consumed per day were compared to families with non-smoking adults. The authors concluded that higher cigarette consumption was associated with increased predisposition for acute respiratory illness. In a paediatric characterisation study of 76 patients with acute rhinosinusitis aged 4-18 years, Eyigör and Başak (63) reported that 51.3% (39 patients) were exposed to second hand smoke and 2.6% (2 patients) were active smokers. Based on their population, the authors concluded that exposure to primary or second hand smoke were predisposing factors for ARS. In a study characterising the respiratory symptoms of adult postal workers in Zagreb, Croatia, the prevalence of sinusitis in 15 Supplement 23 active smokers was 53.1% compared to 26.4% in non-smokers, although no information was available on whether the sinusitis was recurrent acute or chronic in nature (99).
Active smokers with on-going allergic inflammation have an increased susceptibility to ARS compared to non-smokers with on-going allergic inflammation, suggesting that exposure to cigarette smoke and allergic inflammation is mediated via different and possibly synergistic mechanisms. Research to elucidate these mechanisms is needed.
The impact of second-hand tobacco smoke on symptoms of rhinosinusitis has also been evaluated in patients with AR (100). This study reported that patients with AR exposed to second hand smoke had more symptoms consistent with rhinosinusitis including facial pain and facial congestion or fullness, and a greater proportion had received medication for rhinosinusitis including antibiotics for respiratory problems in the previous 12 weeks compared to disease specific controls. Although the authors did not evaluate the occurrences of ARS, the greater proportion of patients requiring antibiotics for respiratory problems would suggest that patients exposed to second-hand tobacco smoke may have had more episodes of ARS or recurrent ARS, although the authors do not delineate between antibiotics for upper or lower airway respiratory problems. Active and passive smoking has been shown to alter the normal bacterial flora present in the nasopharyngeal spaces, resulting in the colonisation of more potential pathogens than found in non-smokers (101). Following smoking cessation, the microbial population has been shown to revert back to that found in nonsmokers (102). The impact of smoking cessation programmes on the incidence and prevalence of ARS is unknown.
In vitro and in vivo studies have recently shown to increased MMP-9 production in children exposed to passive smokers (85) and increased complement activation in human respiratory epithelial cells and mice exposed to cigarette smoke extract (103). Whether increased MMP-9 production or complement activation due to exposure to cigarette smoke predisposes to ARS is unknown and requires further investigation.
3.1.2.7. Laryngopharyngeal reflux
Little is known about the association of ARS and laryngopharyngeal reflux. As reviewed by Pacheco-Galván et al. (104), epidemiological studies conducted between 1997 and 2006 have shown significant associations between GERD and sinusitis. However, in a recent systematic review, Flook and Kumar showed only a poor association between acid reflux, nasal symptoms, and ARS (105).
3.1.2.8. Anxiety and depression
Poor mental health or anxiety and depression have been significantly associated with ARS (106). In a study of 47,202 college students aged 18 to 24 years, Adams et al. (106) reported that the prevalence of acute infectious illness, which included bronchitis, ear infection, sinusitis, and strep throat, ranged from 8% to 29%, while the prevalence of anxiety and depression ranged were 12% to 20%, respectively.
Poor mental health, anxiety, or depression is associated with susceptibility to ARS, although the underlying mechanisms are unclear.
3.1.2.9. Drug resistance
The most common bacterial pathogens causing acute bacterial rhinosinusitis include S. pneumoniae, H. influenzae, S. pyrogenes M. Catarrhalis, and S aureus (8). Amoxicillin/clavulanate is the principal antibiotic for the treatment of mild ARS. Despite resistance to amoxicillin, it is estimated that approximately 80% of cases of mild ARS respond to amoxicillin, at a dose of 70-90 mg/kg/day. Indeed, Principi and Esposito report that most cases of H. influenzae and M. catharralis and approximately 15% of S. pneumoniae resolve spontaneously (107).
Amoxicillin is the most commonly used antibiotic for mild ARS. However, increasing resistance to amoxicillin, particularly in S. pneumoniae and H. influenzae infections need to be reviewed with caution. Furthermore, changes in bacterial pathogenicity in acute bacterial rhinosinusitis require consideration for antibiotic therapy.
The introduction of the Pneumococcal conjugate vaccine has led to changes in the pathogen profile of ARS. Brook and Gober (108) reported a reduction in the incidence of S. pneumoniae from 44% to 27%, and an increase in the incidence of H. influenzae from 37% to 44%, S. pyrogenes from 7% to 12% and S. aureus from 4% to 8% with no change in M. catarrhalis (from 13% to 14%).
Since the introduction of the Pneumococcal conjugate vaccine (PCV7), reductions in the frequency of S. pneumoniae, overall resistance and high level bacterial resistance have been coupled with indications for increasing levels of β-lactamase-producing H. influenza (109). However, evidence of increasing antibiotic resistance in non-PCV7 serotypes of S. pneumoniae is emerging (110). Rybak (111) reported for the US element of the PROTEKT longitudinal global surveillance study on antibiotic resistance, that for 2000-2001, S. pneumoniae resistance to beta-lactams, macrolides and fluoroquinolone, but not to telithromycin. 16 European Position Paper on Rhinosinusitis and Nasal Polyps 2012 In 2004, Huang et al. reported that 72.4% S. pneumonia, 60.5% H. influenzae, and 58.3% M. catarrhalis resistance to first-line antibiotics. Sahm et al. (112) report that 40% of 847 sinus isolates were resistant to two or more of the antibiotics tested, and a doubling of the resistance to amoxicillin/clavulanate. In 2011, Lin et al. (76) report that 70% of isolates of S. pneumoniae and 71.4% of H. influenzae isolates from 69 children were resistant to amoxicillin/clavulanate.
Changes in bacterial pathogenicity in acute bacterial rhinosinusitis require consideration for antibiotic therapy.
Children with chronic disease who develop influenza-like symptoms should be monitored for bacterial ARS. The impact of chronic disease on the likelihood to develop ARS in adults is unknown.
3.1.2.10. Concomitant Chronic Disease
Concomitant chronic disease (bronchitis, asthma, cardiovascular disease, diabetes mellitus, or malignant cancer) in children has been associated with an increased risk of developing ARS secondary to influenza.
Loughlin et al. (113) reported that the overall incidence rate of developing ARS following influenza ranged from 0.9 to 1.3 in children aged 0 to 14 years. While the incidence of ARS subsequent to influenza in healthy children aged 5-14 years was 1.2 (95% CI: 0.9 – 1.5), this increased to 3.1 (95% CI: 1.5 – 5.8) in children with chronic disease (rate ratio: 2.7 (95% CI: 1.5 – 5.4). Increased monitoring of children with chronic disease who develop influenza maybe necessary
3.2. Pathophysiology of ARS
Summary
Acute rhinosinusitis is a common disorder and it could be divided into acute viral rhinosinusitis and acute bacterial rhinosinusitis and is often preceded by a viral rhinitis or common cold. This study reviews the inflammatory mechanisms underlying viral rhinitis, acute viral rhinosinusitis and acute bacterial rhinosinusitis. First of all, the host needs to recognize the presence of microorganisms through 'pattern recognition', initiating the host defense mechanisms through activation of multiple signal pathways. Host defense mechanisms consist of both cellular immune responses and release of soluble chemical factors, which operate in the body through a complex interaction with cytokines and other mediators.
3.2.1. Viral ARS (common cold), post-viral ARS, and bacterial ARS: a continuum?
ARS could be divided theoretically into viral (common cold), post-viral and bacterial ARS (ABRS) and they usually appear in this consecutive order. However, viral, post-viral, and bacterial ARS show a considerable overlap both in their inflammatory mechanism as in their clinical presentation. Viral infection of the nose and sinuses induces multiple changes, including post-viral inflammation, which increase the risk of bacterial superinfection. These changes include epithelial damage and mechanical, humoral, and cellular defences.
ARS can be induced by viral and by bacterial infections.
3.2.2. Microbiology of viral (common cold), postviral, and bacterial ARS
Acute bacterial rhinosinusitis (ABRS) is generally preceded by a viral and or post-viral ARS.
Poor mental health or anxiety and depression have been significantly associated with ARS (106). In a study of 47,202 college students aged 18 to 24 years, Adams et al. (106) reported that the prevalence of acute infectious illness, which included bronchitis, ear infection, sinusitis, and strep throat, ranged from 8% to 29%, while the prevalence of anxiety and depression ranged were 12% to 20%, respectively.
Poor mental health, anxiety, or depression is associated with susceptibility to ARS, although the underlying mechanisms are unclear.
3.1.2.9. Drug resistance
The most common bacterial pathogens causing acute bacterial rhinosinusitis include S. pneumoniae, H. influenzae, S. pyrogenes M. Catarrhalis, and S aureus (8). Amoxicillin/clavulanate is the principal antibiotic for the treatment of mild ARS. Despite resistance to amoxicillin, it is estimated that approximately 80% of cases of mild ARS respond to amoxicillin, at a dose of 70-90 mg/kg/day. Indeed, Principi and Esposito report that most cases of H. influenzae and M. catharralis and approximately 15% of S. pneumoniae resolve spontaneously (107).
Amoxicillin is the most commonly used antibiotic for mild ARS. However, increasing resistance to amoxicillin, particularly in S. pneumoniae and H. influenzae infections need to be reviewed with caution. Furthermore, changes in bacterial pathogenicity in acute bacterial rhinosinusitis require consideration for antibiotic therapy.
The introduction of the Pneumococcal conjugate vaccine has led to changes in the pathogen profile of ARS. Brook and Gober (108) reported a reduction in the incidence of S. pneumoniae from 44% to 27%, and an increase in the incidence of H. influenzae from 37% to 44%, S. pyrogenes from 7% to 12% and S. aureus from 4% to 8% with no change in M. catarrhalis (from 13% to 14%).
Since the introduction of the Pneumococcal conjugate vaccine (PCV7), reductions in the frequency of S. pneumoniae, overall resistance and high level bacterial resistance have been coupled with indications for increasing levels of β-lactamase-producing H. influenza (109). However, evidence of increasing antibiotic resistance in non-PCV7 serotypes of S. pneumoniae is emerging (110). Rybak (111) reported for the US element of the PROTEKT longitudinal global surveillance study on antibiotic resistance, that for 2000-2001, S. pneumoniae resistance to beta-lactams, macrolides and fluoroquinolone, but not to telithromycin. 16 European Position Paper on Rhinosinusitis and Nasal Polyps 2012 In 2004, Huang et al. reported that 72.4% S. pneumonia, 60.5% H. influenzae, and 58.3% M. catarrhalis resistance to first-line antibiotics. Sahm et al. (112) report that 40% of 847 sinus isolates were resistant to two or more of the antibiotics tested, and a doubling of the resistance to amoxicillin/clavulanate. In 2011, Lin et al. (76) report that 70% of isolates of S. pneumoniae and 71.4% of H. influenzae isolates from 69 children were resistant to amoxicillin/clavulanate.
Changes in bacterial pathogenicity in acute bacterial rhinosinusitis require consideration for antibiotic therapy.
Children with chronic disease who develop influenza-like symptoms should be monitored for bacterial ARS. The impact of chronic disease on the likelihood to develop ARS in adults is unknown.
3.1.2.10. Concomitant Chronic Disease
Concomitant chronic disease (bronchitis, asthma, cardiovascular disease, diabetes mellitus, or malignant cancer) in children has been associated with an increased risk of developing ARS secondary to influenza.
Loughlin et al. (113) reported that the overall incidence rate of developing ARS following influenza ranged from 0.9 to 1.3 in children aged 0 to 14 years. While the incidence of ARS subsequent to influenza in healthy children aged 5-14 years was 1.2 (95% CI: 0.9 – 1.5), this increased to 3.1 (95% CI: 1.5 – 5.8) in children with chronic disease (rate ratio: 2.7 (95% CI: 1.5 – 5.4). Increased monitoring of children with chronic disease who develop influenza maybe necessary
3.2. Pathophysiology of ARS
Summary
Acute rhinosinusitis is a common disorder and it could be divided into acute viral rhinosinusitis and acute bacterial rhinosinusitis and is often preceded by a viral rhinitis or common cold. This study reviews the inflammatory mechanisms underlying viral rhinitis, acute viral rhinosinusitis and acute bacterial rhinosinusitis. First of all, the host needs to recognize the presence of microorganisms through 'pattern recognition', initiating the host defense mechanisms through activation of multiple signal pathways. Host defense mechanisms consist of both cellular immune responses and release of soluble chemical factors, which operate in the body through a complex interaction with cytokines and other mediators.
3.2.1. Viral ARS (common cold), post-viral ARS, and bacterial ARS: a continuum?
ARS could be divided theoretically into viral (common cold), post-viral and bacterial ARS (ABRS) and they usually appear in this consecutive order. However, viral, post-viral, and bacterial ARS show a considerable overlap both in their inflammatory mechanism as in their clinical presentation. Viral infection of the nose and sinuses induces multiple changes, including post-viral inflammation, which increase the risk of bacterial superinfection. These changes include epithelial damage and mechanical, humoral, and cellular defences.
ARS can be induced by viral and by bacterial infections.
3.2.2. Microbiology of viral (common cold), postviral, and bacterial ARS
- Viruses
Acute bacterial rhinosinusitis (ABRS) is generally preceded by a viral and or post-viral ARS.
- Bacteria
3.2.3. Inflammatory mechanisms in viral (common cold),
post-viral, and bacterial ARS
3.2.3.1. Invasion of microorganisms into the host
A variety of physical and biochemical barriers prevent entry from infectious agents into the body. First of all, the human body contains a variety of physical barriers against entry of microorganisms. Most important are the skin and airway mucosa. Epithelial cells are the first barrier in contact with viruses or bacteria. These release and express mediators and receptors to initiate elimination mechanisms. Mucus secretion by goblet cells prevents adherence of micro-organisms to the epithelial cells, thus preventing their entrance into the body. Microorganisms become trapped in the mucus and are mechanically removed from the airway by ciliary movements of ciliated cells (118).
Second, the human ecosystem performs a selection of potential microorganisms. The ecosystem is determined by multiple parameters such as temperature, pH, or O2 tension. Only microorganisms that require an ecosystem that is similar to that of the internal environment of the human body are able to survive and infect human (118).
Viral infection of the nose and sinuses induces multiple changes, which increase the risk of bacterial superinfection.
Rhinoviruses, for example, infect airway epithelial cells through binding on ICAM-1 receptors on de cell surface (120, 121). This is followed by penetration of the virus into the cell and replication of the viral RNA (122, 123). The expression of ICAM-1 is upregulated by the rhinoviruses itself, via IL-1beta and nuclear factor (NF)-ΚBdependent mechanisms, thereby enhancing its own infectivity and promoting inflammatory cell infiltration (120, 122, 124). Bianco et al. showed that ICAM-1 expression is enhanced by the Th2 cytokine IL-13 in the atopic airway (125). Whereas in rhinovirus infection down regulates ICAM-1 levels on the infected cells, decreasing the available cellular binding sites for viral attachment and limiting host infectivity (121).
ABRS is mainly caused by: Streptococcus pneumoniae, Haemophilus influenza, Moraxella catarrhalis, and Staphylococcus aureus.
Viral infection of the nasal tissue may also directly increase bacterial adhesion to the nasal epithelial cells. Wang et al. noticed a significant increased adhesion of S. aureus, S. pneumoniae, and H. influenza on rhinovirus-infected cells (132). They postulated that the increased expression of host cell adhesion molecules in the nasal epithelial cells, after rhinovirus infection, may be the mechanism for the increased susceptibility to ABRS associated with rhinovirus-induced upper respiratory infections (132).
Other studies confirmed preferential association and cooperation between viruses and bacteria, for example Influenza A virus and Streptococcal infection, and Human Rhinovirus 14 and S. pneumoniae (133). The mechanism of this superinfection may be in relation to viral replication, which increases bacterial adhesion.
A variety of physical and biochemical barriers prevent entry from infectious agents into the noses and sinuses.
Next to host factors, also bacterial factors are involved in bacterial superinfection. S. pneumoniae and H. influenza are pathogenic because of the structure of their capsule, which gives them an invasive activity. Other bacteria, for example Streptococci, Staphylococci and Gram-negative bacteria, produce toxins directed against the defence system, leukocytes or epithelial cells, which allows easier invasion and development (119).
3.2.3.1. Invasion of microorganisms into the host
A variety of physical and biochemical barriers prevent entry from infectious agents into the body. First of all, the human body contains a variety of physical barriers against entry of microorganisms. Most important are the skin and airway mucosa. Epithelial cells are the first barrier in contact with viruses or bacteria. These release and express mediators and receptors to initiate elimination mechanisms. Mucus secretion by goblet cells prevents adherence of micro-organisms to the epithelial cells, thus preventing their entrance into the body. Microorganisms become trapped in the mucus and are mechanically removed from the airway by ciliary movements of ciliated cells (118).
Second, the human ecosystem performs a selection of potential microorganisms. The ecosystem is determined by multiple parameters such as temperature, pH, or O2 tension. Only microorganisms that require an ecosystem that is similar to that of the internal environment of the human body are able to survive and infect human (118).
- Viruses
Viral infection of the nose and sinuses induces multiple changes, which increase the risk of bacterial superinfection.
Rhinoviruses, for example, infect airway epithelial cells through binding on ICAM-1 receptors on de cell surface (120, 121). This is followed by penetration of the virus into the cell and replication of the viral RNA (122, 123). The expression of ICAM-1 is upregulated by the rhinoviruses itself, via IL-1beta and nuclear factor (NF)-ΚBdependent mechanisms, thereby enhancing its own infectivity and promoting inflammatory cell infiltration (120, 122, 124). Bianco et al. showed that ICAM-1 expression is enhanced by the Th2 cytokine IL-13 in the atopic airway (125). Whereas in rhinovirus infection down regulates ICAM-1 levels on the infected cells, decreasing the available cellular binding sites for viral attachment and limiting host infectivity (121).
- Bacteria
ABRS is mainly caused by: Streptococcus pneumoniae, Haemophilus influenza, Moraxella catarrhalis, and Staphylococcus aureus.
Viral infection of the nasal tissue may also directly increase bacterial adhesion to the nasal epithelial cells. Wang et al. noticed a significant increased adhesion of S. aureus, S. pneumoniae, and H. influenza on rhinovirus-infected cells (132). They postulated that the increased expression of host cell adhesion molecules in the nasal epithelial cells, after rhinovirus infection, may be the mechanism for the increased susceptibility to ABRS associated with rhinovirus-induced upper respiratory infections (132).
Other studies confirmed preferential association and cooperation between viruses and bacteria, for example Influenza A virus and Streptococcal infection, and Human Rhinovirus 14 and S. pneumoniae (133). The mechanism of this superinfection may be in relation to viral replication, which increases bacterial adhesion.
A variety of physical and biochemical barriers prevent entry from infectious agents into the noses and sinuses.
Next to host factors, also bacterial factors are involved in bacterial superinfection. S. pneumoniae and H. influenza are pathogenic because of the structure of their capsule, which gives them an invasive activity. Other bacteria, for example Streptococci, Staphylococci and Gram-negative bacteria, produce toxins directed against the defence system, leukocytes or epithelial cells, which allows easier invasion and development (119).
3.2.3.2. Defence systems of the host, after penetration of
microorganisms into the body
3.2.3.2.1. General principles
If microorganisms succeed to enter the body, two main defensive strategies against the infection come into play. First a non-specific phase where the mucus and its contents (for example lysozyme, lactoferrin, and defensin) play a major role (innate immunity). The second including the immune response and inflammatory reaction (addaptive immunity).
3.2.3.2.2. Pattern recognition and Toll-like receptors.
In order to work properly, the immune system must be able to recognize microbial patterns and differentiate these from molecular structures present on host cells. Specific pathogen classes express class specific molecules, the pathogen associated molecular patterns (PAMP). Activation of PAMP receptors, for example Toll-like receptors (TLR), induces multiple signal cascades, involving complement activation, haemostasis, phagocytosis, inflammation, and apoptosis, in response to pathogens. For example, activation of TLR-dependent signalling pathways contributes to activation of the adaptive immune response, through the expression of effector molecules such as inflammatory cytokines, chemokines, and other co-stimulatory molecules (135-137).
In human, ten distinct TLRs have been described. These are expressed in various combinations in cells of the immune system, as well as in other cell types (138). mRNA of all ten TLRs has been described in human nasal airway tissue. Protein verification however, is still lacking for most TLRs in the nose (139). Corresponding proteins have been documented for TLR-2, TLR3, TLR-4 and TLR-5 (140).
Another well-known PAMP in bacteria is lipopolysaccharide (LPS), which is part of the outer membrane of Gram-negative bacteria. LPS induced activation of TLR-4 pathways, causing increased transcription of nuclear factor-NF-ΚB genes, which regulated genes like those encoding cytokines and chemokines. (149-151). This enhances the microbicidal activity of phagocytic cells and stimulates maturation and migration of dendritic cells. These mature dendritic cells show an increased antigenpresenting capacity and are involved in the activation of the adaptive immune response by stimulation of T lymphocytes. Thus, the TLR-4 signalling pathway forms a critical link between innate and adaptive immune responses (152, 153).
In S. pneumoniae infection, also lipoteichoic acid and pneumolysin have been shown to initiate inflammatory responses. This occurs through activation of the TLR-2 pathway. The TLR-2 pathway is shown to contribute to the adaptive, rather than the innate immune responses, by expression of co-stimulatory molecules and molecules such as MHC-II which are necessary to present bacterial antigens to Th cells. Cytokines that result from the TLR-2 pathway, stimulate a Th1 response, which is very important to clear pneumococcal colonization (154-157). It has been suggested that pneumolysin can also interact with TLR-4, inducing innate immune responses to pneumococci. However, Van Rossum et al found no confirmation of a role of TLR-4 in the clearance of pneumococcal colonization in their murine model (156, 158).
3.2.3.2.3. Soluble chemical factors
3.2.3.2.3.1. Defensin, lysozyme, C-reactive protein and the complement system
As mentioned above, the first defensive strategy of the host against infection consists of a non-specific phase, where the mucus and its contents (for example defensin and lysozyme) play a major role. Other important soluble chemical factors are acute phase proteins such as C-reactive protein, interferon, lactoferrin, sIgA, and the complement system (159).
3.2.3.2.3.2. Kinins
3.2.3.2.1. General principles
If microorganisms succeed to enter the body, two main defensive strategies against the infection come into play. First a non-specific phase where the mucus and its contents (for example lysozyme, lactoferrin, and defensin) play a major role (innate immunity). The second including the immune response and inflammatory reaction (addaptive immunity).
- Viruses
- Bacteria
3.2.3.2.2. Pattern recognition and Toll-like receptors.
In order to work properly, the immune system must be able to recognize microbial patterns and differentiate these from molecular structures present on host cells. Specific pathogen classes express class specific molecules, the pathogen associated molecular patterns (PAMP). Activation of PAMP receptors, for example Toll-like receptors (TLR), induces multiple signal cascades, involving complement activation, haemostasis, phagocytosis, inflammation, and apoptosis, in response to pathogens. For example, activation of TLR-dependent signalling pathways contributes to activation of the adaptive immune response, through the expression of effector molecules such as inflammatory cytokines, chemokines, and other co-stimulatory molecules (135-137).
In human, ten distinct TLRs have been described. These are expressed in various combinations in cells of the immune system, as well as in other cell types (138). mRNA of all ten TLRs has been described in human nasal airway tissue. Protein verification however, is still lacking for most TLRs in the nose (139). Corresponding proteins have been documented for TLR-2, TLR3, TLR-4 and TLR-5 (140).
- Viruses
- Bacteria
Another well-known PAMP in bacteria is lipopolysaccharide (LPS), which is part of the outer membrane of Gram-negative bacteria. LPS induced activation of TLR-4 pathways, causing increased transcription of nuclear factor-NF-ΚB genes, which regulated genes like those encoding cytokines and chemokines. (149-151). This enhances the microbicidal activity of phagocytic cells and stimulates maturation and migration of dendritic cells. These mature dendritic cells show an increased antigenpresenting capacity and are involved in the activation of the adaptive immune response by stimulation of T lymphocytes. Thus, the TLR-4 signalling pathway forms a critical link between innate and adaptive immune responses (152, 153).
In S. pneumoniae infection, also lipoteichoic acid and pneumolysin have been shown to initiate inflammatory responses. This occurs through activation of the TLR-2 pathway. The TLR-2 pathway is shown to contribute to the adaptive, rather than the innate immune responses, by expression of co-stimulatory molecules and molecules such as MHC-II which are necessary to present bacterial antigens to Th cells. Cytokines that result from the TLR-2 pathway, stimulate a Th1 response, which is very important to clear pneumococcal colonization (154-157). It has been suggested that pneumolysin can also interact with TLR-4, inducing innate immune responses to pneumococci. However, Van Rossum et al found no confirmation of a role of TLR-4 in the clearance of pneumococcal colonization in their murine model (156, 158).
3.2.3.2.3. Soluble chemical factors
3.2.3.2.3.1. Defensin, lysozyme, C-reactive protein and the complement system
As mentioned above, the first defensive strategy of the host against infection consists of a non-specific phase, where the mucus and its contents (for example defensin and lysozyme) play a major role. Other important soluble chemical factors are acute phase proteins such as C-reactive protein, interferon, lactoferrin, sIgA, and the complement system (159).
- Viruses
- Bacteria
3.2.3.2.3.2. Kinins
- Viruses
- Bacteria
3.2.3.2.3.3. Nitric oxide (NO)
NO is a gaseous molecule, synthesized by NO synthase (NOS), an enzyme that catalyses the oxidation of L-arginine to NO and L-citrulline. At least two types of NOS can be reported, constitutive NOS (cNOS) and inducible NOS (iNOS) (168). cNOS is produced by many cells in the upper and lower respiratory system, such as parasympathetic vasodilator nerves, endothelial cells and ciliated mucosa cells (169). iNOS is described in epithelium, macrophages, fibroblasts, neutrophils, endothelium and vascular smooth muscle, and is activated by proinflammatory cytokines and endotoxins (168, 170, 171). NO is involved in many physiological and pathological processes in human, by exerting a role as cellular signalling molecule. Its actions in the body include vasoregulation, haemostasis, neurotransmission, immune defence, and respiration (168). In the respiratory airway, it causes smooth muscle relaxation, affects ciliary beat frequency, mucus secretion and plasma exudation, and it is involved in neurotransmission, inflammation and cellmediated immunity (172).
In patients with rhinosinusitis, on the contrary, the levels of nasal NO (nNO) are significantly decreased. These reduced levels of nNO are likely because of reduced NO flow into the nasal lumen due to mucosal swelling and draining ostia obstruction, and removal of NO by reactive oxygen species (168, 176, 177). It is 20 European Position Paper on Rhinosinusitis and Nasal Polyps 2012 thought that the lack of NO may contribute to the pathogenesis of sinusitis.
3.2.3.2.4. Nerve stimulation and neuromediators
Sympathetic nerve stimulation induces vasoconstriction and consequent decreases nasal airway resistance. Parasympathetic nerve stimulation on the other hand, promotes secretion from nasal airway glands and nasal congestion. The nasal mucosa also contains nerves of the non-adrenergic, non-cholinergic (NANC)- system. Neuropeptides from the latter nerves (substance P, neurokinin A and K, and calcitonin gene-related peptide) are suspected to play a role in vasodilatation, mucus secretion, plasma extravasation, neurogenic inflammation, and mast cell nerve interactions. However, the magnitude of their role is uncertain (179). Further investigations concerning the role of the nervous system in ARS are required.
3.2.3.2.5. Cell-mediated immune response
In addition to the non-specific defence consisting of barriers and soluble chemical factors, a cell-mediated immune response is activated
3.2.3.2.5.1. Phagocytosis - neutrophils, monocytes and macrophages
The innate immune system operates through phagocytosis of the microorganisms. Cells with phagocytic capacity are neutrophils, monocytes, and macrophages.
3.2.3.2.5.2. Antigen presentation - Dendritic cells
The adaptive immune system becomes activated in specific stimulus. Specific antigens are presented to T lymphocytes (cytotoxic T cells, as well as T helper cells) by antigen-presenting cells, such as monocytes, macrophages, B-lymphocytes, and dendritic cells. In the peripheral blood, two major subtypes of dendritic cells are identified, myeloid dendritic cells (MDC), and plasmacytoid dendritic cells (PDC) (182). Hartmann et al. demonstrated the presence of PDC and MDC in the healthy nasal epithelium and in nasal epithelia from patients with different pathological conditions (183). Antigen-presenting cells need to process the complex protein antigens into 'minimal antigenic peptides', which are presented to T cells on appropriate MHC molecules. Binding of this complex (antigenic peptide and MHC molecule) on the antigenspecific T cell receptor, initiates activation of the adaptive immunity (184).
The adaptive immune system generates an adequate immune response to a specific stimulus (antigen-presenting cells, T lymphocytes, B lymphocytes, and plasma cells).
3.2.3.2.5.3. Specific immunity – T lymphocytes and B lymphocytes
The adaptive immunity reacts on antigen presentation through formation of immune products (effector T lymphocytes and antibodies), which can generate a specific interaction with the stimulus.
NO is a gaseous molecule, synthesized by NO synthase (NOS), an enzyme that catalyses the oxidation of L-arginine to NO and L-citrulline. At least two types of NOS can be reported, constitutive NOS (cNOS) and inducible NOS (iNOS) (168). cNOS is produced by many cells in the upper and lower respiratory system, such as parasympathetic vasodilator nerves, endothelial cells and ciliated mucosa cells (169). iNOS is described in epithelium, macrophages, fibroblasts, neutrophils, endothelium and vascular smooth muscle, and is activated by proinflammatory cytokines and endotoxins (168, 170, 171). NO is involved in many physiological and pathological processes in human, by exerting a role as cellular signalling molecule. Its actions in the body include vasoregulation, haemostasis, neurotransmission, immune defence, and respiration (168). In the respiratory airway, it causes smooth muscle relaxation, affects ciliary beat frequency, mucus secretion and plasma exudation, and it is involved in neurotransmission, inflammation and cellmediated immunity (172).
- Viruses
In patients with rhinosinusitis, on the contrary, the levels of nasal NO (nNO) are significantly decreased. These reduced levels of nNO are likely because of reduced NO flow into the nasal lumen due to mucosal swelling and draining ostia obstruction, and removal of NO by reactive oxygen species (168, 176, 177). It is 20 European Position Paper on Rhinosinusitis and Nasal Polyps 2012 thought that the lack of NO may contribute to the pathogenesis of sinusitis.
- Bacteria
3.2.3.2.4. Nerve stimulation and neuromediators
Sympathetic nerve stimulation induces vasoconstriction and consequent decreases nasal airway resistance. Parasympathetic nerve stimulation on the other hand, promotes secretion from nasal airway glands and nasal congestion. The nasal mucosa also contains nerves of the non-adrenergic, non-cholinergic (NANC)- system. Neuropeptides from the latter nerves (substance P, neurokinin A and K, and calcitonin gene-related peptide) are suspected to play a role in vasodilatation, mucus secretion, plasma extravasation, neurogenic inflammation, and mast cell nerve interactions. However, the magnitude of their role is uncertain (179). Further investigations concerning the role of the nervous system in ARS are required.
3.2.3.2.5. Cell-mediated immune response
In addition to the non-specific defence consisting of barriers and soluble chemical factors, a cell-mediated immune response is activated
3.2.3.2.5.1. Phagocytosis - neutrophils, monocytes and macrophages
The innate immune system operates through phagocytosis of the microorganisms. Cells with phagocytic capacity are neutrophils, monocytes, and macrophages.
- Viruses
- Bacteria
3.2.3.2.5.2. Antigen presentation - Dendritic cells
The adaptive immune system becomes activated in specific stimulus. Specific antigens are presented to T lymphocytes (cytotoxic T cells, as well as T helper cells) by antigen-presenting cells, such as monocytes, macrophages, B-lymphocytes, and dendritic cells. In the peripheral blood, two major subtypes of dendritic cells are identified, myeloid dendritic cells (MDC), and plasmacytoid dendritic cells (PDC) (182). Hartmann et al. demonstrated the presence of PDC and MDC in the healthy nasal epithelium and in nasal epithelia from patients with different pathological conditions (183). Antigen-presenting cells need to process the complex protein antigens into 'minimal antigenic peptides', which are presented to T cells on appropriate MHC molecules. Binding of this complex (antigenic peptide and MHC molecule) on the antigenspecific T cell receptor, initiates activation of the adaptive immunity (184).
- Viruses
- Bacteria
The adaptive immune system generates an adequate immune response to a specific stimulus (antigen-presenting cells, T lymphocytes, B lymphocytes, and plasma cells).
3.2.3.2.5.3. Specific immunity – T lymphocytes and B lymphocytes
The adaptive immunity reacts on antigen presentation through formation of immune products (effector T lymphocytes and antibodies), which can generate a specific interaction with the stimulus.
- Viruses
- Bacteria
3.2.3.2.6. Cytokines and other mediators
Multiple mediators and cytokines orchestrate the migration and activation of immune effector cells in response to infection. These proteins regulate chemotaxis, cellular differentiation and activation, by induction of adhesion molecule expression and by release of cytokines (180).
IL-1beta has a dual effect. It increases rhinovirus spread via ICAM-1 upregulation and initiates the host response to infection by enhancing the recruitment of immune effector cells into the inflammation site. It also induces the release of proinflammatory cytokines such as platelet activating factor and IL-8 (179, 200-202).
IL-6 is a proinflammatory cytokine, which has activating and proliferating effects on lymphocytes. IL-8, on the other hand, is a strong chemo-attractant for neutrophils (124, 180). IL-10 is a regulatory cytokine with anti-inflammatory and Th2 stimulating properties. It can regulate immune responses by either preventing an inflammatory response or by limiting excessive ongoing inflammation, though inhibition of production of a wide range of other cytokines. For example, Th1-related cytokines (TNF-alpha, IFN-gamma, IL-2, and IL-12), proinflammatory cytokine IL-18, and Th2-related cytokine I-5 (203).
TNF-alpha is also a Th1-related cytokines. It induces activation of the antiviral host immune response through the stimulation of functional activities of cytotoxic T lymphocytes, NK cells and macrophages, and through the recruitment of inflammatory cells to the site of infection. Moreover, together with IL-12, it can promote the development of Th1 lymphocytes (203). In allergic individuals, experimental rhinovirus infection also induces increase of granulocyte colony-stimulating factor (G-CSF) in nasal secretions and serum. G-CSF and IL-8 were rapidly induced in the nose after viral inoculation, and appeared to be related to neutrophil trafficking in the airway. Concerning G-CSF, it is suggested that either G-CSF contributes to neutrophil recruitment to the airway, or that airway neutrophils are a source of G-CSF during viral infection. Increases in nasal G-CSF also correlated with increases in blood neutrophils, suggesting that G-CSF produced in the nose enters the systemic circulation and acts on the bone marrow to increase neutrophilia in the blood (204, 205). However, Linden et al. confirmed that G-CSF is only elevated in virus-infected patients with concomitant allergic rhinitis and not in non-allergic individuals (206).
Multiple mediators and cytokines orchestrate the migration and activation of immune effector cells in response to infection. These proteins regulate chemotaxis, cellular differentiation and activation, by induction of adhesion molecule expression and by release of cytokines (180).
- Viruses
IL-1beta has a dual effect. It increases rhinovirus spread via ICAM-1 upregulation and initiates the host response to infection by enhancing the recruitment of immune effector cells into the inflammation site. It also induces the release of proinflammatory cytokines such as platelet activating factor and IL-8 (179, 200-202).
IL-6 is a proinflammatory cytokine, which has activating and proliferating effects on lymphocytes. IL-8, on the other hand, is a strong chemo-attractant for neutrophils (124, 180). IL-10 is a regulatory cytokine with anti-inflammatory and Th2 stimulating properties. It can regulate immune responses by either preventing an inflammatory response or by limiting excessive ongoing inflammation, though inhibition of production of a wide range of other cytokines. For example, Th1-related cytokines (TNF-alpha, IFN-gamma, IL-2, and IL-12), proinflammatory cytokine IL-18, and Th2-related cytokine I-5 (203).
TNF-alpha is also a Th1-related cytokines. It induces activation of the antiviral host immune response through the stimulation of functional activities of cytotoxic T lymphocytes, NK cells and macrophages, and through the recruitment of inflammatory cells to the site of infection. Moreover, together with IL-12, it can promote the development of Th1 lymphocytes (203). In allergic individuals, experimental rhinovirus infection also induces increase of granulocyte colony-stimulating factor (G-CSF) in nasal secretions and serum. G-CSF and IL-8 were rapidly induced in the nose after viral inoculation, and appeared to be related to neutrophil trafficking in the airway. Concerning G-CSF, it is suggested that either G-CSF contributes to neutrophil recruitment to the airway, or that airway neutrophils are a source of G-CSF during viral infection. Increases in nasal G-CSF also correlated with increases in blood neutrophils, suggesting that G-CSF produced in the nose enters the systemic circulation and acts on the bone marrow to increase neutrophilia in the blood (204, 205). However, Linden et al. confirmed that G-CSF is only elevated in virus-infected patients with concomitant allergic rhinitis and not in non-allergic individuals (206).
- Bacteria
3.2.4. Allergy and ARS
As mentioned above, there exists a pathophysiological link between AR and rhinosinusitis (130).
Skoner et al. compared the systemic cellular immune responses to experimental rhinovirus challenge in AR and non-AR subjects (212). They found that rhinovirus infection induced significant acute increases in serum IgE, leucocyte histamine release and platelet aggregation, but caused no changes in serum IgE, serum IgA, serum IgM, and plasma histamine. This change was confined to the AR subjects, but there was no evidence that the acute rise in total serum IgE was due to an elevation of a preexisting, pollen-specific serum IgE antibody (213). Alho et al. studied the cellular and structural changes in the nasal mucosa during natural colds in subjects with AR and susceptibility to recurrent sinusitis, compared to healthy controls. They demonstrated that allergic subjects had elevated levels of eosinophils in the acute phase compared to the control group. The allergic and sinusitis-prone subjects also had elevated levels of epithelial T cells and low levels of mast cells in convalescence compared to the control group. In convalescence, the allergic subjects also had the highest numbers of intraepithelial cytotoxic lymphocytes, while such cells were absent in the sinusitis-prone subjects. The delayed accumulation of intraepithelial T cells could indicate a prolonged inflammatory reaction in the allergic and sinusitis-prone subjects, compared to the control subjects. They hypothesized that this late response of T cells consists of virus-specific T cells. The higher level of cytotoxic lymphocytes in allergic subjects during convalescence may be related to the more severe mucosal changes in the paranasal sinuses that have previously been shown in subjects with AR during viral colds (214).
As mentioned above, there exists a pathophysiological link between AR and rhinosinusitis (130).
- Viruses
Skoner et al. compared the systemic cellular immune responses to experimental rhinovirus challenge in AR and non-AR subjects (212). They found that rhinovirus infection induced significant acute increases in serum IgE, leucocyte histamine release and platelet aggregation, but caused no changes in serum IgE, serum IgA, serum IgM, and plasma histamine. This change was confined to the AR subjects, but there was no evidence that the acute rise in total serum IgE was due to an elevation of a preexisting, pollen-specific serum IgE antibody (213). Alho et al. studied the cellular and structural changes in the nasal mucosa during natural colds in subjects with AR and susceptibility to recurrent sinusitis, compared to healthy controls. They demonstrated that allergic subjects had elevated levels of eosinophils in the acute phase compared to the control group. The allergic and sinusitis-prone subjects also had elevated levels of epithelial T cells and low levels of mast cells in convalescence compared to the control group. In convalescence, the allergic subjects also had the highest numbers of intraepithelial cytotoxic lymphocytes, while such cells were absent in the sinusitis-prone subjects. The delayed accumulation of intraepithelial T cells could indicate a prolonged inflammatory reaction in the allergic and sinusitis-prone subjects, compared to the control subjects. They hypothesized that this late response of T cells consists of virus-specific T cells. The higher level of cytotoxic lymphocytes in allergic subjects during convalescence may be related to the more severe mucosal changes in the paranasal sinuses that have previously been shown in subjects with AR during viral colds (214).
- Bacteria
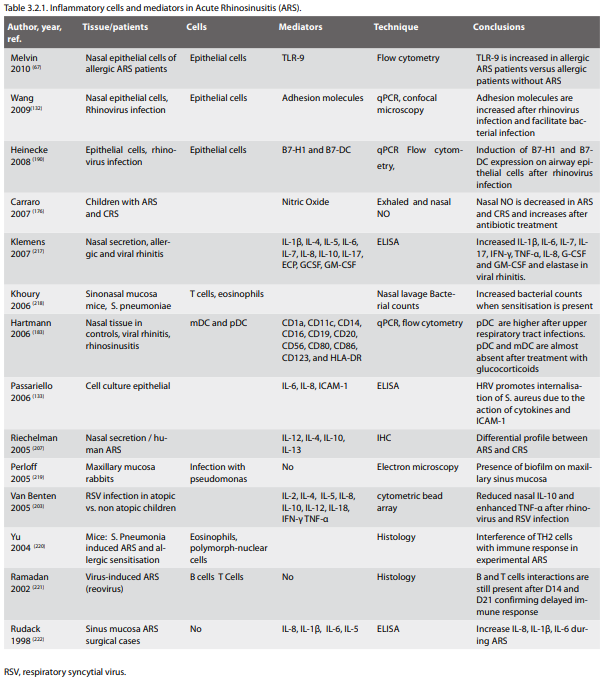
3.3. Diagnosis and Differential Diagnosis of ARS
Summary
ARS is a common condition that is often self-managed by patients without medical care being sought, and will usually improve spontaneously or with treatment. When patients do consult, this is usually to generalist primary care clinicians. The diagnosis is clinical and relies on the presence and duration of typical symptoms, particularly nasal blockage, discharge, facial pain or pressure and reduction in smell. ARS usually occurs as a complication of a viral acute upper respiratory tract infection, with persistence of symptoms beyond 10 days or worsening of symptoms after 5 days. Persistence of symptoms beyond 12 weeks signifies chronic rather than acute rhinosinusitis. Differentiation from other conditions such as viral URTI, allergic rhinitis, oro-dental disease and facial pain syndromes should be possible in most cases on clinical grounds, although investigations may be needed when diagnostic doubt remains. Septic complications are rare but serious, and all primary care clinicians should be aware of 'red flag' symptoms such as periorbital oedema and visual symptoms, which require urgent specialist assessment. Although antibiotics are commonly prescribed in community practice, ARS the symptoms of ARS often relate more to inflammation and disruption of sinus drainage mechanisms, and in most cases antibiotics is not required. Imaging, haematological and microbiological investigations and endoscopy are not routinely required in the diagnosis of ARS, but may be needed in particular settings, such as research studies or in high-risk patients.
3.3.1. Introduction
Post-viral ARS is a common condition in the community, usually following viral URTI.
ARS is a common condition, and is usually self-limiting. Many patients will self-manage or use over the counter remedies, so will not seek medical care or have a formal diagnosis made. When medical care is sought, most patients will consult with a primary care physician, although in some health systems may directly access specialist services. Although educational efforts have been made to familiarize General Practitioners (GPs) with the concepts of rhinosinusitis and the diagnostic criteria for the diagnosis of ARS (223), 'sinusitis' is commonly used as a diagnostic label, and as this is frequently considered by GPs an acute bacterial rather than inflammatory condition (224), antibiotics are extensively prescribed (225, 226). The dissemination of the EP3 OS (8) and other recent guidelines (2, 227) emphasizing the inflammatory nature of ARS and providing standardization of diagnostic criteria and use of investigations has lead to more rational diagnosis and management in some (226, 228) but not all (229, 230) settings. In addition to misunderstandings concerning the inflammatory nature of ARS (229), concern over the risk of septic complications from untreated bacterial disease may be a factor in the ongoing high use of antibiotics in ARS. Observational evidence indicates, however, that complications are rare (231, 232) usually manifest early in the course of the illness with severe symptoms (233, 234), and that antibiotic treatment of ARS in general practice does not prevent complications (52, 232). Guidelines agree that in uncomplicated cases, ARS is diagnosed on clinical criteria and supplementary investigations are not required (2). In particular patient groups and in those with severe or atypical symptoms, additional diagnostic procedures may be needed, as discussed below. ARS is frequently an isolated clinical event and a self-limiting condition, although may be recurrent in some cases. There may be an association with dental disease in some (61).
3.3.2. Clinical Diagnosis in Primary Care
ARS is diagnosed by the acute onset of typical symptoms that include nasal blockage, discharge, facial pain or pressure and reduction in smell.
In primary care setting (and for epidemiological research), ARS is defined by symptomatology without detailed ENT examination or imaging. ARS is defined in section 2 of this guideline by the presence of major and minor symptoms for up to 12 weeks. ARS is sub-divided into 'acute viral rhinosinusitis' (synonymous with the 'common cold'), in which the duration of symptoms is less than 10 days, usually a self-limiting condition that frequently does not present to clinicians, and 'acute post-viral rhinosinusitis', defined by an increase in symptoms after 5 days or persistence beyond 10 days (8).
3.3.2.1. Assessment of ARS symptoms
Most acute viral URTI infections are self-limiting, and post-viral ARS should not diagnosed before 10 days duration of symptoms unless there is a clear worsening of symptoms after 5 days.
3.3.2.1.1. Symptoms of ARS
The subjective assessment of ARS is based on the presence and severity of symptoms.
• Nasal blockage, congestion or stuffiness
• Nasal discharge or postnasal drip, often mucopurulent
• Facial pain or pressure, headache, and
• Reduction/loss of smell
Besides these local symptoms, distant and systemic symptoms may occur.
Distant symptoms are pharyngeal, laryngeal, and tracheal irritation causing sore throat, dysphonia, and cough, and general symptoms including drowsiness, malaise, and fever. There is little reliable evidence of the relative frequency of different symptoms in ARS in community practice. Individual variations of these general symptom patterns are many (235-239). Only a small proportion of patients with purulent rhinosinusitis, without coexisting chest disease, complain of cough (236). In patients with a suspicion of infection, facial or dental pain (especially if unilateral) have been found to be predictors of acute maxillary sinusitis, when validated by maxillary antral aspiration (236) or paranasal sinus radiographs (237)..The symptoms of ARS occur abruptly without a history of recent nasal or sinus symptoms. A history of sudden worsening of preexisting symptoms suggests an acute exacerbation of chronic rhinosinusitis, which should be diagnosed by similar criteria and treated in a similar way to ARS.
3.3.2.1.2. Subjective assessment of symptoms: severity
Subjective assessment should address the severity and the duration of symptoms. The recommended method of assessing severity of symptoms is with the use of a visual analogue scale (VAS) recorded by the patient on a 10cm line giving a score on a measurable continuum of 1 to 10 (see chapter 2.2.3.). Diseasespecific questionnaires measuring quality of life impairment are available (240, 241) but not commonly used in clinical practice; a good clinician will, however, informally assess the impact of ARS on their patient as part of a full clinical assessment. The VAS can be used to assess overall symptom severity and the severity of individual symptoms (see below). Asking patients to rate their symptoms as absent, mild, moderate or severe, may also assess symptom severity.
3.3.2.1.3. Subjective assessment of symptoms: duration
The sudden onset of symptoms of nasal blockage, obstruction, congestion and discharge is usually due to a self limiting viral infection, and ARS should not be considered in patients who have experience symptoms for less than 5 days unless they are unusually severe. Post-viral ARS should not be diagnosed in patients with symptoms for less than 10 days unless a marked worsening of symptoms occurs after 5 days, and features of severe pain and a pyrexia of >38°C are present. Symptoms occurring for longer than 12 weeks indicate the presence of chronic rhinosinusitis.
3.3.2.1.4. Assessment of specific individual symptoms
3.3.2.1.4.1. Individual symptoms
Nasal obstruction. Although nasal obstruction can be assessed objectively with techniques such as rhinomanometry, nasal peak inspiratory flow and acoustic rhinometry, these are rarely used in the diagnosis and assessment of ARS, which relies on patient report of obstruction and subjective assessment of severity, either by VAS score or by assessing obstruction as absent, mild, moderate or severe.
3.3.2.1.4.2. Individual symptoms: Nasal discharge
The presence and severity of nasal discharge (anterior or posterior nasal drip) is assessed by subjective report, and graded by VAS score or by patient subjective assessment as absent, mild, moderate or severe. Patient reported purulence of nasal discharge has been recommended as a diagnostic criterion for acute bacterial rhinosinusitis (227), and is prioritized by GPs as a feature indicating the need for antibiotics (226), with limited evidence to support this. Purulent nasal secretions have been reported to increase the likelihood ratio of radiological sinus opacity (237), and of obtaining a positive bacterial culture (242), although purulent rhinorrhoea with a unilateral predominance has a positive predictive value (PPV) of only 50%, and pus in the nasal cavity a PPV of only 17%, in the prediction of a positive bacterial culture of an aspirate of the maxillary sinus (236), so cannot be relied upon to accurately identify bacterial infection.
3.3.2.1.4.3. Individual symptoms: Smell abnormalities
Reduction of smell can be rated by patient subjective report as a VAS score or assessed as absent, mild, moderate, or severe. Subjective report of olfaction correlates well with objective tests (243-245) and loss of olfaction is commonly associated with ARS.
3.3.2.1.4.4. Individual symptoms: Facial pain and pressure
Facial pain and pressure commonly occur in ARS, although may also occur transiently in self-limiting viral upper respiratory tract infection (URTI). Facial or dental pain, especially when unilateral, has been found to be a predictor of acute maxillary sinusitis with fluid retention in patients with suspected bacterial infection when confirmed by maxillary antral aspiration (236) or paranasal sinus radiographs (237). Pain on bending forwards and maxillary toothache, particularly when unilateral, are often interpreted by GPs as indicative of more severe disease and the need for antibiotics (226), with limited supportive evidence. Maxillary toothache is reported to increase the likelihood ratio of radiological sinus opacity to 2.5 (237), although the PPV of local unilateral pain for bacterial infection was only 41% in another study (236). A further study reported that maxillary toothache was significantly associated with the presence of a positive bacteriological culture, predominantly of S. pneumoniae or H. influenzae, obtained by sinus aspiration or lavage (246).The severity of pain can be rated subjectively by patients as a VAS score or as absent, mild, moderate, or severe.
Bacterial infection may occur in ARS, but in most cases antibiotics have little effect on the course of the illness.
3.3.2.1.5. Clinical rules for the prediction of bacterial disease
A number of studies have attempted to provide clinicians with combinations of symptoms and signs predicting more severe disease, particularly in the prediction of a bacterial infection and the likelihood of a response to antibiotics. In a study of primary care patients aged 15 years or older with a clinical diagnosis of ARS which assessed the likelihood of specific symptoms and tests in predicting a fluid level or total opacity of any sinus on CT (as a gold standard of sinusitis), Lindbaek (247) reported four factors having a high likelihood ratio and independently associated with ARS. These were purulent rhinorrhoea, purulent secretion in cavum nasi, a raised ESR (>10), and 'double sickening' (i.e. a deterioration after an initial milder phase of illness). A combination of at least three of these four symptoms and signs gave a specificity of 0.81 and a sensitivity of 0.66 for ARS.
Berg (236) reported that 2 or more positive findings (from purulent rhinorrhoea with unilateral predominance, local pain with unilateral predominance, pus in the nasal cavity and bilateral purulent rhinorrhoea) provided 95% sensitivity and 77% specificity for ABRS. Williams (237) reported that fewer than 2 symptoms (from maxillary toothache, poor response to antihistamines or decongestants, purulent nasal secretions, abnormal transillumination and coloured nasal discharge) ruled out ABRS with a positive predictive value (PPV) of <40%, and 4 or more symptoms ruled in ABRS (PPV, 81%).
Summary
ARS is a common condition that is often self-managed by patients without medical care being sought, and will usually improve spontaneously or with treatment. When patients do consult, this is usually to generalist primary care clinicians. The diagnosis is clinical and relies on the presence and duration of typical symptoms, particularly nasal blockage, discharge, facial pain or pressure and reduction in smell. ARS usually occurs as a complication of a viral acute upper respiratory tract infection, with persistence of symptoms beyond 10 days or worsening of symptoms after 5 days. Persistence of symptoms beyond 12 weeks signifies chronic rather than acute rhinosinusitis. Differentiation from other conditions such as viral URTI, allergic rhinitis, oro-dental disease and facial pain syndromes should be possible in most cases on clinical grounds, although investigations may be needed when diagnostic doubt remains. Septic complications are rare but serious, and all primary care clinicians should be aware of 'red flag' symptoms such as periorbital oedema and visual symptoms, which require urgent specialist assessment. Although antibiotics are commonly prescribed in community practice, ARS the symptoms of ARS often relate more to inflammation and disruption of sinus drainage mechanisms, and in most cases antibiotics is not required. Imaging, haematological and microbiological investigations and endoscopy are not routinely required in the diagnosis of ARS, but may be needed in particular settings, such as research studies or in high-risk patients.
3.3.1. Introduction
Post-viral ARS is a common condition in the community, usually following viral URTI.
ARS is a common condition, and is usually self-limiting. Many patients will self-manage or use over the counter remedies, so will not seek medical care or have a formal diagnosis made. When medical care is sought, most patients will consult with a primary care physician, although in some health systems may directly access specialist services. Although educational efforts have been made to familiarize General Practitioners (GPs) with the concepts of rhinosinusitis and the diagnostic criteria for the diagnosis of ARS (223), 'sinusitis' is commonly used as a diagnostic label, and as this is frequently considered by GPs an acute bacterial rather than inflammatory condition (224), antibiotics are extensively prescribed (225, 226). The dissemination of the EP3 OS (8) and other recent guidelines (2, 227) emphasizing the inflammatory nature of ARS and providing standardization of diagnostic criteria and use of investigations has lead to more rational diagnosis and management in some (226, 228) but not all (229, 230) settings. In addition to misunderstandings concerning the inflammatory nature of ARS (229), concern over the risk of septic complications from untreated bacterial disease may be a factor in the ongoing high use of antibiotics in ARS. Observational evidence indicates, however, that complications are rare (231, 232) usually manifest early in the course of the illness with severe symptoms (233, 234), and that antibiotic treatment of ARS in general practice does not prevent complications (52, 232). Guidelines agree that in uncomplicated cases, ARS is diagnosed on clinical criteria and supplementary investigations are not required (2). In particular patient groups and in those with severe or atypical symptoms, additional diagnostic procedures may be needed, as discussed below. ARS is frequently an isolated clinical event and a self-limiting condition, although may be recurrent in some cases. There may be an association with dental disease in some (61).
3.3.2. Clinical Diagnosis in Primary Care
ARS is diagnosed by the acute onset of typical symptoms that include nasal blockage, discharge, facial pain or pressure and reduction in smell.
In primary care setting (and for epidemiological research), ARS is defined by symptomatology without detailed ENT examination or imaging. ARS is defined in section 2 of this guideline by the presence of major and minor symptoms for up to 12 weeks. ARS is sub-divided into 'acute viral rhinosinusitis' (synonymous with the 'common cold'), in which the duration of symptoms is less than 10 days, usually a self-limiting condition that frequently does not present to clinicians, and 'acute post-viral rhinosinusitis', defined by an increase in symptoms after 5 days or persistence beyond 10 days (8).
3.3.2.1. Assessment of ARS symptoms
Most acute viral URTI infections are self-limiting, and post-viral ARS should not diagnosed before 10 days duration of symptoms unless there is a clear worsening of symptoms after 5 days.
3.3.2.1.1. Symptoms of ARS
The subjective assessment of ARS is based on the presence and severity of symptoms.
• Nasal blockage, congestion or stuffiness
• Nasal discharge or postnasal drip, often mucopurulent
• Facial pain or pressure, headache, and
• Reduction/loss of smell
Besides these local symptoms, distant and systemic symptoms may occur.
Distant symptoms are pharyngeal, laryngeal, and tracheal irritation causing sore throat, dysphonia, and cough, and general symptoms including drowsiness, malaise, and fever. There is little reliable evidence of the relative frequency of different symptoms in ARS in community practice. Individual variations of these general symptom patterns are many (235-239). Only a small proportion of patients with purulent rhinosinusitis, without coexisting chest disease, complain of cough (236). In patients with a suspicion of infection, facial or dental pain (especially if unilateral) have been found to be predictors of acute maxillary sinusitis, when validated by maxillary antral aspiration (236) or paranasal sinus radiographs (237)..The symptoms of ARS occur abruptly without a history of recent nasal or sinus symptoms. A history of sudden worsening of preexisting symptoms suggests an acute exacerbation of chronic rhinosinusitis, which should be diagnosed by similar criteria and treated in a similar way to ARS.
3.3.2.1.2. Subjective assessment of symptoms: severity
Subjective assessment should address the severity and the duration of symptoms. The recommended method of assessing severity of symptoms is with the use of a visual analogue scale (VAS) recorded by the patient on a 10cm line giving a score on a measurable continuum of 1 to 10 (see chapter 2.2.3.). Diseasespecific questionnaires measuring quality of life impairment are available (240, 241) but not commonly used in clinical practice; a good clinician will, however, informally assess the impact of ARS on their patient as part of a full clinical assessment. The VAS can be used to assess overall symptom severity and the severity of individual symptoms (see below). Asking patients to rate their symptoms as absent, mild, moderate or severe, may also assess symptom severity.
3.3.2.1.3. Subjective assessment of symptoms: duration
The sudden onset of symptoms of nasal blockage, obstruction, congestion and discharge is usually due to a self limiting viral infection, and ARS should not be considered in patients who have experience symptoms for less than 5 days unless they are unusually severe. Post-viral ARS should not be diagnosed in patients with symptoms for less than 10 days unless a marked worsening of symptoms occurs after 5 days, and features of severe pain and a pyrexia of >38°C are present. Symptoms occurring for longer than 12 weeks indicate the presence of chronic rhinosinusitis.
3.3.2.1.4. Assessment of specific individual symptoms
3.3.2.1.4.1. Individual symptoms
Nasal obstruction. Although nasal obstruction can be assessed objectively with techniques such as rhinomanometry, nasal peak inspiratory flow and acoustic rhinometry, these are rarely used in the diagnosis and assessment of ARS, which relies on patient report of obstruction and subjective assessment of severity, either by VAS score or by assessing obstruction as absent, mild, moderate or severe.
3.3.2.1.4.2. Individual symptoms: Nasal discharge
The presence and severity of nasal discharge (anterior or posterior nasal drip) is assessed by subjective report, and graded by VAS score or by patient subjective assessment as absent, mild, moderate or severe. Patient reported purulence of nasal discharge has been recommended as a diagnostic criterion for acute bacterial rhinosinusitis (227), and is prioritized by GPs as a feature indicating the need for antibiotics (226), with limited evidence to support this. Purulent nasal secretions have been reported to increase the likelihood ratio of radiological sinus opacity (237), and of obtaining a positive bacterial culture (242), although purulent rhinorrhoea with a unilateral predominance has a positive predictive value (PPV) of only 50%, and pus in the nasal cavity a PPV of only 17%, in the prediction of a positive bacterial culture of an aspirate of the maxillary sinus (236), so cannot be relied upon to accurately identify bacterial infection.
3.3.2.1.4.3. Individual symptoms: Smell abnormalities
Reduction of smell can be rated by patient subjective report as a VAS score or assessed as absent, mild, moderate, or severe. Subjective report of olfaction correlates well with objective tests (243-245) and loss of olfaction is commonly associated with ARS.
3.3.2.1.4.4. Individual symptoms: Facial pain and pressure
Facial pain and pressure commonly occur in ARS, although may also occur transiently in self-limiting viral upper respiratory tract infection (URTI). Facial or dental pain, especially when unilateral, has been found to be a predictor of acute maxillary sinusitis with fluid retention in patients with suspected bacterial infection when confirmed by maxillary antral aspiration (236) or paranasal sinus radiographs (237). Pain on bending forwards and maxillary toothache, particularly when unilateral, are often interpreted by GPs as indicative of more severe disease and the need for antibiotics (226), with limited supportive evidence. Maxillary toothache is reported to increase the likelihood ratio of radiological sinus opacity to 2.5 (237), although the PPV of local unilateral pain for bacterial infection was only 41% in another study (236). A further study reported that maxillary toothache was significantly associated with the presence of a positive bacteriological culture, predominantly of S. pneumoniae or H. influenzae, obtained by sinus aspiration or lavage (246).The severity of pain can be rated subjectively by patients as a VAS score or as absent, mild, moderate, or severe.
Bacterial infection may occur in ARS, but in most cases antibiotics have little effect on the course of the illness.
3.3.2.1.5. Clinical rules for the prediction of bacterial disease
A number of studies have attempted to provide clinicians with combinations of symptoms and signs predicting more severe disease, particularly in the prediction of a bacterial infection and the likelihood of a response to antibiotics. In a study of primary care patients aged 15 years or older with a clinical diagnosis of ARS which assessed the likelihood of specific symptoms and tests in predicting a fluid level or total opacity of any sinus on CT (as a gold standard of sinusitis), Lindbaek (247) reported four factors having a high likelihood ratio and independently associated with ARS. These were purulent rhinorrhoea, purulent secretion in cavum nasi, a raised ESR (>10), and 'double sickening' (i.e. a deterioration after an initial milder phase of illness). A combination of at least three of these four symptoms and signs gave a specificity of 0.81 and a sensitivity of 0.66 for ARS.
Berg (236) reported that 2 or more positive findings (from purulent rhinorrhoea with unilateral predominance, local pain with unilateral predominance, pus in the nasal cavity and bilateral purulent rhinorrhoea) provided 95% sensitivity and 77% specificity for ABRS. Williams (237) reported that fewer than 2 symptoms (from maxillary toothache, poor response to antihistamines or decongestants, purulent nasal secretions, abnormal transillumination and coloured nasal discharge) ruled out ABRS with a positive predictive value (PPV) of <40%, and 4 or more symptoms ruled in ABRS (PPV, 81%).
3.3.2.2. Clinical examination
3.3.2.2.1. Anterior rhinoscopy
Although anterior rhinoscopy alone is a very limited investigation, it should be performed in primary care setting as part of the clinical assessment of suspected ARS. It may reveal supportive findings such as nasal inflammation, mucosal oedema and purulent nasal discharge, and can sometimes reveal previously unsuspected findings such as polyps or anatomical abnormalities.
3.3.2.2.2. Temperature
The presence of a fever of >38°C indicates the presence of a more severe illness and the possible need for more active treatment, particularly in conjunction with more severe symptoms. A fever of >38°C is significantly associated with the presence of a positive bacteriologic culture, predominantly S. pneumoniae and H. influenzae, obtained by sinus aspiration or lavage (246).
3.3.2.2.3. Inspection and palpation of sinuses
Inspection and palpation of the maxillofacial area can reveal swelling and tenderness, which are commonly interpreted as indicating more severe disease (226) and the need for antibiotics, although the sensitivity and specificity of this symptom in the identification of ABRS is not established.
3.3.2.2.4. Nasal endoscopy
Nasal endoscopy is not generally available in routine primary care settings, and is not required in the clinical diagnosis of ARS, although may be required in research settings, and is discussed below.
3.3.2.3. Additional Investigations
3.3.2.3.1. Bacteriology
Microbiological investigations are not required for the diagnosis of ARS in routine practice, although may be required in research settings, or in atypical or recurrent disease. There is a reasonable correlation between specimens taken from the middle meatus under endoscopic control and sinus taps (248), and microbiological sampling may be indicated in more severe, recurrent or complicated presentations
3.3.2.3.2. Imaging
Imaging studies and not required in the diagnosis of ARS in routine practice, although may be required to confirm the diagnosis in research settings, and are discussed further below
3.3.2.3.3. C-Reactive Protein (CRP)
CRP is a haematological biomarker (available as rapid assay near-patient testing kits) and is raised in bacterial infection. Its use has been advocated in respiratory tract infection (247) as an aid to targeting bacterial infection and so in limiting unnecessary antibiotic use. Recent studies (249, 250) have suggested that in ARS, a low or normal CRP may identify patients with a low likelihood of positive bacterial infection who are unlikely to need or benefit from antibiotics, and CRP guided treatment has been associated with a reduction in antibiotic use without any impairment of outcomes. This can be regarded as an interesting but preliminary observation, and more research is needed before this test can be recommended as routine in the diagnosis of ARS and in the targeting of therapy. However, CRP levels are significantly correlated with changes in CT scans (251) and a raised CRP is predictive of a positive bacterial culture on sinus puncture or lavage (246, 252).
3.3.2.3.4. Procalcitonin
Procalcitonin has also been advocated as a potential haematological biomarker indicating more severe bacterial infection, and investigated as a tool for guiding antibiotic prescribing in respiratory tract infections in the community (253). It is available as a near-patient manual assay that can provide results in 30 minutes, but with limited performance results (254), or as a laboratory test. At present, however, there is no evidence of its effectiveness as a biomarker in ARS
3.3.2.3.5. Erythrocyte Sedimentation Rate (ESR) and plasma viscosity
Markers of inflammation such as ESR and plasma viscosity are raised in ARS, may reflect disease severity and can indicate the need for more aggressive treatment in a similar way to CRP. ERS levels are correlated with CT changes in ARS (251) and an ESR of >10 is predictive of sinus fluid levels or sinus opacity on CT scans (252). A raised ESR is predictive of a positive bacterial culture on sinus puncture or lavage (246, 252).
3.3.2.3.6. Nasal Nitric Oxide (NO)
This gaseous metabolite is found in the upper and lower respiratory tract and is a sensitive indicator of the presence of inflammation and ciliary dysfunction. Measurement of nasal NO is relatively simple, requires simple patient co-operation by exhaling into the analyser, and is quick and easy to perform using chemiluminescence assay equipment. Measurement is feasible in routine clinical settings, and as the technology improves and cost of measurement apparatus reduces, may be practicable as a clinical tool. Preliminary evidence exists of feasibility of using exhaled NO measurement in primary care in asthma diagnosis and monitoring (255), but the feasibility of use of nasal NO in routine care has not been assessed. Very low levels of nasal NO may indicate primary ciliary dyskinesia, but may also occur insignificant sinus obstruction (256). Elevated levels may suggest the presence of inflammation provided ostiomeatal patency is maintained. A recent pilot study (257) has suggested that monitoring of nasal NO levels may be useful in the diagnosis and management of ARS, but further research is needed.
3.3.2.3.7. Other investigations
Detailed tests of nasal airway function such as tests of mucociliary function, nasal patency, and olfaction are rarely performed in the diagnosis of ARS other than in specific research settings.
3.3.2.4. Differential Diagnosis of ARS in clinical practice
The symptoms of ARS are non-specific and may overlap with a number of other conditions, which should be differentiated.
3.3.2.4.1. Viral Upper Respiratory Tract Infection (URTI)
The symptoms of the common cold and of self-limiting viral URTIs overlap with those of post-viral ARS. Indeed, most episodes of ARS will start as a viral URTI, but with a prolonged illness beyond 10 days or with worsening symptoms after 5 days. Most common colds are associated with rhinovirus infection with symptoms peaking by 3 days (258), and the majority of patients do not seek medical care. The diagnosis is clinical and supportive advice, symptomatic treatment and reassurance are generally the only interventions required.
3.3.2.4.2. Allergic rhinitis
Allergic rhinitis (AR) is a common global condition affecting 10-20% of the adult population (259). Allergic rhinitis is the most common form of non-infectious rhinitis and is associated with an IgE-mediated immune response against allergens, and is often associated with ocular symptoms. Since the nasal mucosa is continuous with that of the paranasal sinuses, congestion of the ostia may result in sinusitis, which does not exist without rhinitis, so AR may be part of an allergic rhinosinusitis with similar symptoms to those of ARS (and CRS). Symptoms of AR include rhinorrhoea (non-purulent), nasal obstruction, nasal itching, and sneezing, which are reversible spontaneously or with treatment. AR is subdivided into "intermittent" or "persistent" disease. Intermittent rhinitis may occur suddenly in response to exposure to a specific allergen, and so cause diagnostic confusion between AR and ARS. Seasonal AR is related to a wide variety of outdoor allergens such as pollens or molds, and sudden exposure to such aeroallergens or to others (e.g. cat and dog dander in sensitized individuals) can cause acute onset of symptoms. In AR, there will usually be a history of similar symptoms in response to similar exposures, often with a seasonal pattern. Non-specific irritants such as air pollution and viral infection may aggravate symptoms in symptomatic AR patients and induce symptoms in asymptomatic patients with subclinical nasal inflammation. The diagnosis of AR and differentiation from ARS is made mainly on the basis of a prior history of allergy and atopy, and exposure to an allergen (usually an aeroallergen) to which the patient is sensitized. Ocular symptoms are common in AR, in particular in patients allergic to outdoor allergens, but not in ARS. Mucopurulent rhinorrhoea, pain, nasal obstruction without other symptoms and anosmia are uncommon in AR. Diagnostic tests for AR are based on the demonstration of allergen-specific IgE in the skin (skin tests) or the blood (specific IgE), and may be considered to clarify the diagnosis, particularly in those with severe or persistent symptoms.
3.3.2.4.3. Orodontal disease
Patients with orodontal disease may present to primary care physicians with ill-defined facial pain, with or without fever and toothache. The absence of other ARS-associated symptoms such as rhinorrhoea, nasal discharge and smell disturbance will make ARS a less likely diagnosis, although in some cases doubt may persist. A dental assessment and dental radiography may be required to clarify the diagnosis. ARS may occur more frequently and have overlapping symptoms in patients with orodental disease (61).
3.3.2.4.4. Rare diseases
A number of less common conditions may occasionally present acutely with similar symptoms to ARS.
3.3.2.4.4.1. Intracranial sepsis
Intracranial sepsis is uncommon but it is crucial that primary care practitioners are aware of the warning signs of complicated and severe illness and refer promptly when the diagnosis is possible. Symptoms such as periorbital oedema, displaced globe, diplopia, ophtalmoplegia, reduced visual acuity, severe unilateral or bilateral frontal headache, frontal headache, focal neurological signs or meningism point to complications such as intracranial sepsis, or an alternative diagnosis and requite urgent diagnosis and appropriate management. (See Table 3.3.1)
3.3.2.2.1. Anterior rhinoscopy
Although anterior rhinoscopy alone is a very limited investigation, it should be performed in primary care setting as part of the clinical assessment of suspected ARS. It may reveal supportive findings such as nasal inflammation, mucosal oedema and purulent nasal discharge, and can sometimes reveal previously unsuspected findings such as polyps or anatomical abnormalities.
3.3.2.2.2. Temperature
The presence of a fever of >38°C indicates the presence of a more severe illness and the possible need for more active treatment, particularly in conjunction with more severe symptoms. A fever of >38°C is significantly associated with the presence of a positive bacteriologic culture, predominantly S. pneumoniae and H. influenzae, obtained by sinus aspiration or lavage (246).
3.3.2.2.3. Inspection and palpation of sinuses
Inspection and palpation of the maxillofacial area can reveal swelling and tenderness, which are commonly interpreted as indicating more severe disease (226) and the need for antibiotics, although the sensitivity and specificity of this symptom in the identification of ABRS is not established.
3.3.2.2.4. Nasal endoscopy
Nasal endoscopy is not generally available in routine primary care settings, and is not required in the clinical diagnosis of ARS, although may be required in research settings, and is discussed below.
3.3.2.3. Additional Investigations
3.3.2.3.1. Bacteriology
Microbiological investigations are not required for the diagnosis of ARS in routine practice, although may be required in research settings, or in atypical or recurrent disease. There is a reasonable correlation between specimens taken from the middle meatus under endoscopic control and sinus taps (248), and microbiological sampling may be indicated in more severe, recurrent or complicated presentations
3.3.2.3.2. Imaging
Imaging studies and not required in the diagnosis of ARS in routine practice, although may be required to confirm the diagnosis in research settings, and are discussed further below
3.3.2.3.3. C-Reactive Protein (CRP)
CRP is a haematological biomarker (available as rapid assay near-patient testing kits) and is raised in bacterial infection. Its use has been advocated in respiratory tract infection (247) as an aid to targeting bacterial infection and so in limiting unnecessary antibiotic use. Recent studies (249, 250) have suggested that in ARS, a low or normal CRP may identify patients with a low likelihood of positive bacterial infection who are unlikely to need or benefit from antibiotics, and CRP guided treatment has been associated with a reduction in antibiotic use without any impairment of outcomes. This can be regarded as an interesting but preliminary observation, and more research is needed before this test can be recommended as routine in the diagnosis of ARS and in the targeting of therapy. However, CRP levels are significantly correlated with changes in CT scans (251) and a raised CRP is predictive of a positive bacterial culture on sinus puncture or lavage (246, 252).
3.3.2.3.4. Procalcitonin
Procalcitonin has also been advocated as a potential haematological biomarker indicating more severe bacterial infection, and investigated as a tool for guiding antibiotic prescribing in respiratory tract infections in the community (253). It is available as a near-patient manual assay that can provide results in 30 minutes, but with limited performance results (254), or as a laboratory test. At present, however, there is no evidence of its effectiveness as a biomarker in ARS
3.3.2.3.5. Erythrocyte Sedimentation Rate (ESR) and plasma viscosity
Markers of inflammation such as ESR and plasma viscosity are raised in ARS, may reflect disease severity and can indicate the need for more aggressive treatment in a similar way to CRP. ERS levels are correlated with CT changes in ARS (251) and an ESR of >10 is predictive of sinus fluid levels or sinus opacity on CT scans (252). A raised ESR is predictive of a positive bacterial culture on sinus puncture or lavage (246, 252).
3.3.2.3.6. Nasal Nitric Oxide (NO)
This gaseous metabolite is found in the upper and lower respiratory tract and is a sensitive indicator of the presence of inflammation and ciliary dysfunction. Measurement of nasal NO is relatively simple, requires simple patient co-operation by exhaling into the analyser, and is quick and easy to perform using chemiluminescence assay equipment. Measurement is feasible in routine clinical settings, and as the technology improves and cost of measurement apparatus reduces, may be practicable as a clinical tool. Preliminary evidence exists of feasibility of using exhaled NO measurement in primary care in asthma diagnosis and monitoring (255), but the feasibility of use of nasal NO in routine care has not been assessed. Very low levels of nasal NO may indicate primary ciliary dyskinesia, but may also occur insignificant sinus obstruction (256). Elevated levels may suggest the presence of inflammation provided ostiomeatal patency is maintained. A recent pilot study (257) has suggested that monitoring of nasal NO levels may be useful in the diagnosis and management of ARS, but further research is needed.
3.3.2.3.7. Other investigations
Detailed tests of nasal airway function such as tests of mucociliary function, nasal patency, and olfaction are rarely performed in the diagnosis of ARS other than in specific research settings.
3.3.2.4. Differential Diagnosis of ARS in clinical practice
The symptoms of ARS are non-specific and may overlap with a number of other conditions, which should be differentiated.
3.3.2.4.1. Viral Upper Respiratory Tract Infection (URTI)
The symptoms of the common cold and of self-limiting viral URTIs overlap with those of post-viral ARS. Indeed, most episodes of ARS will start as a viral URTI, but with a prolonged illness beyond 10 days or with worsening symptoms after 5 days. Most common colds are associated with rhinovirus infection with symptoms peaking by 3 days (258), and the majority of patients do not seek medical care. The diagnosis is clinical and supportive advice, symptomatic treatment and reassurance are generally the only interventions required.
3.3.2.4.2. Allergic rhinitis
Allergic rhinitis (AR) is a common global condition affecting 10-20% of the adult population (259). Allergic rhinitis is the most common form of non-infectious rhinitis and is associated with an IgE-mediated immune response against allergens, and is often associated with ocular symptoms. Since the nasal mucosa is continuous with that of the paranasal sinuses, congestion of the ostia may result in sinusitis, which does not exist without rhinitis, so AR may be part of an allergic rhinosinusitis with similar symptoms to those of ARS (and CRS). Symptoms of AR include rhinorrhoea (non-purulent), nasal obstruction, nasal itching, and sneezing, which are reversible spontaneously or with treatment. AR is subdivided into "intermittent" or "persistent" disease. Intermittent rhinitis may occur suddenly in response to exposure to a specific allergen, and so cause diagnostic confusion between AR and ARS. Seasonal AR is related to a wide variety of outdoor allergens such as pollens or molds, and sudden exposure to such aeroallergens or to others (e.g. cat and dog dander in sensitized individuals) can cause acute onset of symptoms. In AR, there will usually be a history of similar symptoms in response to similar exposures, often with a seasonal pattern. Non-specific irritants such as air pollution and viral infection may aggravate symptoms in symptomatic AR patients and induce symptoms in asymptomatic patients with subclinical nasal inflammation. The diagnosis of AR and differentiation from ARS is made mainly on the basis of a prior history of allergy and atopy, and exposure to an allergen (usually an aeroallergen) to which the patient is sensitized. Ocular symptoms are common in AR, in particular in patients allergic to outdoor allergens, but not in ARS. Mucopurulent rhinorrhoea, pain, nasal obstruction without other symptoms and anosmia are uncommon in AR. Diagnostic tests for AR are based on the demonstration of allergen-specific IgE in the skin (skin tests) or the blood (specific IgE), and may be considered to clarify the diagnosis, particularly in those with severe or persistent symptoms.
3.3.2.4.3. Orodontal disease
Patients with orodontal disease may present to primary care physicians with ill-defined facial pain, with or without fever and toothache. The absence of other ARS-associated symptoms such as rhinorrhoea, nasal discharge and smell disturbance will make ARS a less likely diagnosis, although in some cases doubt may persist. A dental assessment and dental radiography may be required to clarify the diagnosis. ARS may occur more frequently and have overlapping symptoms in patients with orodental disease (61).
3.3.2.4.4. Rare diseases
A number of less common conditions may occasionally present acutely with similar symptoms to ARS.
3.3.2.4.4.1. Intracranial sepsis
Intracranial sepsis is uncommon but it is crucial that primary care practitioners are aware of the warning signs of complicated and severe illness and refer promptly when the diagnosis is possible. Symptoms such as periorbital oedema, displaced globe, diplopia, ophtalmoplegia, reduced visual acuity, severe unilateral or bilateral frontal headache, frontal headache, focal neurological signs or meningism point to complications such as intracranial sepsis, or an alternative diagnosis and requite urgent diagnosis and appropriate management. (See Table 3.3.1)
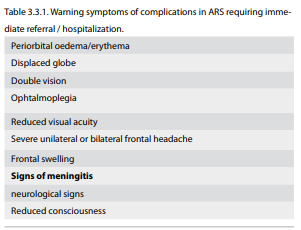
3.3.2.4.4.2. Facial pain syndromes
A number of conditions can present acutely with facial pain and nasal symptoms, including migraine and cluster headaches. The differential diagnosis of facial pain is discussed in section 4. Bilateral pressure sensations without other nasal symptoms may be caused by tension headaches and mid facial segmental pain.
3.3.2.4.4.3. Vasculitis
Autoimmune vasculitides such as Wegener's granulomatosis and Churg-Strauss syndrome or sarcoidosis may involve the nose and sinuses and on rare occasions may present acutely. The presence of other suggestive symptoms and an atypical clinical course can alert the clinician to alternative diagnoses.
3.3.2.4.4.4. Acute invasive fungal rhinosinusitis
In immunosuppressed patients and in (uncontrolled) diabetics, acute invasive fungal rhinosinusitis may present in a similar way to ARS, but with severe and rapidly progressive symptoms (260, 261). When this diagnosis is suspected, a more aggressive diagnostic approach is required as a delay in diagnosis worsens the prognosis.
3.3.2.4.4.5. CSF leak
Unilateral watery rhinorrhoea is uncommon and should raise suspicion of cerebrospinal fluid leakage (262).
3.3.3. Warning signs of complications of ARS
Septic complications of ARS represent a medical emergency and require prompt recognition by generalists and immediate referral to secondary care for assessment (Table 3.3.1).
Septic complications of ARS are uncommon, but vital to identify early. They occur early in the course of the illness and primary care clinicians need to be vigilant for danger signs and symptoms, such as high fever, systemic illness, periorbital oedema and reduced vision
3.3.4. Enhanced Diagnosis in specialist care
Although uncomplicated ARS is more likely to present to primary care physicians, in some health systems patients may present acutely to specialists or may be referred early for a specialist assessment, usually to a rhinologist or ENT specialist. Generally the diagnosis may be made clinically using the same clinical criteria outlined above, but sometimes more detailed diagnostic investigations may be applied. Immediate referral and/or hospitalization are indicated for any of the symptoms listed in table 3.1.1.
3.3.4.1. Nasal endoscopy
Nasal endoscopy may be used to visualize nasal and sinus anatomy and to provide biopsy and microbiological samples. Several microbiology studies (263-267) (Evidence Level IIb) have shown a reasonable correlation between specimens taken from the middle meatus under endoscopic control and proof puncture leading to the possibility of microbiological confirmation of both the pathogen and its response to therapy (Table 3.3.2). A meta-analysis showed an accuracy of 87% with a lower end confidence level of 81.3% for the endoscopically directed middle meatal culture when compared with maxillary sinus taps in acute maxillary sinus infection (248). Some authorities recommend that a clinical diagnosis of acute bacterial rhinosinusitis should always be confirmed by endoscopy and culture (268), as many patients with clinical or radiological evidence of ARS do not have positive bacterial microbiology; since this guideline favours the term 'acute postviral rhinosinusitis', and favours anti-inflammatory rather than anti-infective therapy as first-line management, it is debatable how valid this advice is, particularly in settings where access to endoscopy is limited. Nasal endoscopy is possible in patients of all ages, including children, although does not provide additional information in most (269, 270).
A number of conditions can present acutely with facial pain and nasal symptoms, including migraine and cluster headaches. The differential diagnosis of facial pain is discussed in section 4. Bilateral pressure sensations without other nasal symptoms may be caused by tension headaches and mid facial segmental pain.
3.3.2.4.4.3. Vasculitis
Autoimmune vasculitides such as Wegener's granulomatosis and Churg-Strauss syndrome or sarcoidosis may involve the nose and sinuses and on rare occasions may present acutely. The presence of other suggestive symptoms and an atypical clinical course can alert the clinician to alternative diagnoses.
3.3.2.4.4.4. Acute invasive fungal rhinosinusitis
In immunosuppressed patients and in (uncontrolled) diabetics, acute invasive fungal rhinosinusitis may present in a similar way to ARS, but with severe and rapidly progressive symptoms (260, 261). When this diagnosis is suspected, a more aggressive diagnostic approach is required as a delay in diagnosis worsens the prognosis.
3.3.2.4.4.5. CSF leak
Unilateral watery rhinorrhoea is uncommon and should raise suspicion of cerebrospinal fluid leakage (262).
3.3.3. Warning signs of complications of ARS
Septic complications of ARS represent a medical emergency and require prompt recognition by generalists and immediate referral to secondary care for assessment (Table 3.3.1).
Septic complications of ARS are uncommon, but vital to identify early. They occur early in the course of the illness and primary care clinicians need to be vigilant for danger signs and symptoms, such as high fever, systemic illness, periorbital oedema and reduced vision
3.3.4. Enhanced Diagnosis in specialist care
Although uncomplicated ARS is more likely to present to primary care physicians, in some health systems patients may present acutely to specialists or may be referred early for a specialist assessment, usually to a rhinologist or ENT specialist. Generally the diagnosis may be made clinically using the same clinical criteria outlined above, but sometimes more detailed diagnostic investigations may be applied. Immediate referral and/or hospitalization are indicated for any of the symptoms listed in table 3.1.1.
3.3.4.1. Nasal endoscopy
Nasal endoscopy may be used to visualize nasal and sinus anatomy and to provide biopsy and microbiological samples. Several microbiology studies (263-267) (Evidence Level IIb) have shown a reasonable correlation between specimens taken from the middle meatus under endoscopic control and proof puncture leading to the possibility of microbiological confirmation of both the pathogen and its response to therapy (Table 3.3.2). A meta-analysis showed an accuracy of 87% with a lower end confidence level of 81.3% for the endoscopically directed middle meatal culture when compared with maxillary sinus taps in acute maxillary sinus infection (248). Some authorities recommend that a clinical diagnosis of acute bacterial rhinosinusitis should always be confirmed by endoscopy and culture (268), as many patients with clinical or radiological evidence of ARS do not have positive bacterial microbiology; since this guideline favours the term 'acute postviral rhinosinusitis', and favours anti-inflammatory rather than anti-infective therapy as first-line management, it is debatable how valid this advice is, particularly in settings where access to endoscopy is limited. Nasal endoscopy is possible in patients of all ages, including children, although does not provide additional information in most (269, 270).
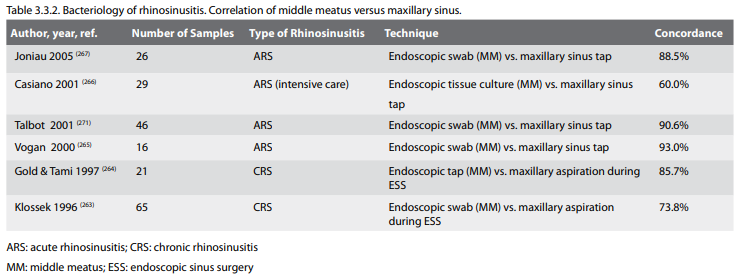
3.3.4.2. Imaging
A number of different imaging modalities are possible in the diagnosis of ARS.
3.3.4.2.1. CT scanning
CT scanning is the imaging modality of choice to confirm the extent of pathology and the anatomy. However, it should not be regarded as the primary step in the diagnosis of the condition, except where there are unilateral signs and symptoms or other sinister signs, but rather corroborates history and endoscopic examination after failure of medical therapy. CT may be considered in very severe disease, in immuno-compromised patients, when there is suspicion of complications. A recent study suggests that routine CT scanning in ARS adds little useful information (251). The demonstration of the complex sinonasal anatomy has however, been regarded as at least as important as confirmation of inflammatory change (272-274). Considerable ethnic as well as individual differences may be encountered (275). Many protocols have been described and interest has recently centered on improving definition whilst reducing radiation dose (276). Incidental abnormalities have been reported on scanning in up to a fifth of the 'normal' population (277), although more recent data have suggested that healthy normal people should not have unexpected abnormal sinus scans (278). In children, in whom plain radiographs are technically difficult, sinus scans are technically possible and are the imaging investigation of choice but similarly are only indicated if complications are suspected or if a lack of response to treatment occurs (279).
3.3.4.2.2. Plain sinus X Rays and transillumination
Plain sinus x-rays are insensitive and of limited usefulness for the diagnosis of rhinosinusitis due to the number of false positive and negative results (280-282). Nevertheless it can be useful to prove ARS in research studies. Transillumination was advocated in the 1970's as an inexpensive and efficacious screening modality for sinus pathology (283). The insensitivity and unspecificity makes it unreliable for the diagnosis of rhinosinusitis (284).
3.3.4.2.3. Ultrasound
Sinus ultrasound is insensitive and of limited usefulness for the diagnosis of ARS due to the number of false positive and negative results. However, the results in well-trained hands are comparable to X-ray in the diagnostics of ARS, and so it may be a useful investigation in some settings (285-287).
3.3.5. ARS diagnosis specific settings
3.3.5.1. Diagnosis for research
In research settings, a more formal diagnosis may be required. In such settings, a variable combination of symptoms, imaging findings, examination findings, and bacteriology samples (obtained from middle meatus or from sinus puncture) may be required for confirmation of the diagnosis as specified in the study protocol. The diagnostic criteria used must be specified in research studies to allow comparison of results between studies.
3.3.5.2. Diagnosis in the intensive care unit
ARS is common in ICU (with risk factors including naso-gastric tubes, mechanical ventilation, failure of defence mechanisms and pronged supine posture), and is associated with poor outcomes. Sepsis may involve multiple sinuses (288). As a consequence, more aggressive diagnostic processes may be appropriate to confirm the diagnosis and to guide treatment. CT scanning may confirm the diagnosis (289), and sinus puncture is safe in skilled hands and can provide important microbiological information to confirm the diagnosis and guide therapy (288).
3.3.5.3. Diagnosis in immunosuppressed patients
Immunosuppressed patients are much more vulnerable to complications of ARS, and a more aggressive diagnostic approach is required. Acute invasive fungal rhinosinusitis (290) is a serious disease with high mortality and morbidity and requires prompt diagnosis and treatment with open or endoscopic sinus surgery. The diagnosis is histopathological, so early endoscopic evaluations indicated, with open biopsy if doubt remains (260, 261).
3.3.6. Recurrent ARS
The differentiation between CRS and recurrent ARS can be difficult, but relies on complete resolution of symptoms and signs between episodes. Some patients do have recurrent episodes of ARS, and may represent a distinct phenotype (291). Such patients should be assessed for underlying risk factor, such as allergy and anatomical abnormalities (60), with consideration of imaging or endoscopic evaluation. Occult immunodeficiency may rarely occur in such patients, but routine screening has a low yield (292).
A number of different imaging modalities are possible in the diagnosis of ARS.
3.3.4.2.1. CT scanning
CT scanning is the imaging modality of choice to confirm the extent of pathology and the anatomy. However, it should not be regarded as the primary step in the diagnosis of the condition, except where there are unilateral signs and symptoms or other sinister signs, but rather corroborates history and endoscopic examination after failure of medical therapy. CT may be considered in very severe disease, in immuno-compromised patients, when there is suspicion of complications. A recent study suggests that routine CT scanning in ARS adds little useful information (251). The demonstration of the complex sinonasal anatomy has however, been regarded as at least as important as confirmation of inflammatory change (272-274). Considerable ethnic as well as individual differences may be encountered (275). Many protocols have been described and interest has recently centered on improving definition whilst reducing radiation dose (276). Incidental abnormalities have been reported on scanning in up to a fifth of the 'normal' population (277), although more recent data have suggested that healthy normal people should not have unexpected abnormal sinus scans (278). In children, in whom plain radiographs are technically difficult, sinus scans are technically possible and are the imaging investigation of choice but similarly are only indicated if complications are suspected or if a lack of response to treatment occurs (279).
3.3.4.2.2. Plain sinus X Rays and transillumination
Plain sinus x-rays are insensitive and of limited usefulness for the diagnosis of rhinosinusitis due to the number of false positive and negative results (280-282). Nevertheless it can be useful to prove ARS in research studies. Transillumination was advocated in the 1970's as an inexpensive and efficacious screening modality for sinus pathology (283). The insensitivity and unspecificity makes it unreliable for the diagnosis of rhinosinusitis (284).
3.3.4.2.3. Ultrasound
Sinus ultrasound is insensitive and of limited usefulness for the diagnosis of ARS due to the number of false positive and negative results. However, the results in well-trained hands are comparable to X-ray in the diagnostics of ARS, and so it may be a useful investigation in some settings (285-287).
3.3.5. ARS diagnosis specific settings
3.3.5.1. Diagnosis for research
In research settings, a more formal diagnosis may be required. In such settings, a variable combination of symptoms, imaging findings, examination findings, and bacteriology samples (obtained from middle meatus or from sinus puncture) may be required for confirmation of the diagnosis as specified in the study protocol. The diagnostic criteria used must be specified in research studies to allow comparison of results between studies.
3.3.5.2. Diagnosis in the intensive care unit
ARS is common in ICU (with risk factors including naso-gastric tubes, mechanical ventilation, failure of defence mechanisms and pronged supine posture), and is associated with poor outcomes. Sepsis may involve multiple sinuses (288). As a consequence, more aggressive diagnostic processes may be appropriate to confirm the diagnosis and to guide treatment. CT scanning may confirm the diagnosis (289), and sinus puncture is safe in skilled hands and can provide important microbiological information to confirm the diagnosis and guide therapy (288).
3.3.5.3. Diagnosis in immunosuppressed patients
Immunosuppressed patients are much more vulnerable to complications of ARS, and a more aggressive diagnostic approach is required. Acute invasive fungal rhinosinusitis (290) is a serious disease with high mortality and morbidity and requires prompt diagnosis and treatment with open or endoscopic sinus surgery. The diagnosis is histopathological, so early endoscopic evaluations indicated, with open biopsy if doubt remains (260, 261).
3.3.6. Recurrent ARS
The differentiation between CRS and recurrent ARS can be difficult, but relies on complete resolution of symptoms and signs between episodes. Some patients do have recurrent episodes of ARS, and may represent a distinct phenotype (291). Such patients should be assessed for underlying risk factor, such as allergy and anatomical abnormalities (60), with consideration of imaging or endoscopic evaluation. Occult immunodeficiency may rarely occur in such patients, but routine screening has a low yield (292).
3.4. Management of ARS
Summary
The introduction of evidence-based management of ARS has a major impact on the physician's management of ARS patients. It has been proven clearly in many clinical studies that ARS resolves without antibiotic treatment in most cases. Symptomatic treatment and reassurance is the preferred initial management strategy for patients with mild symptoms. Intranasal corticosteroids in monotherapy or in adjuvant therapy to oral antibiotics are proven to be effective; however, in patients with severe ARS, oral corticosteroids can be used for short-term relief of headache, facial pain and other acute symptoms. Antibiotic therapy should be reserved for patients with high fever or severe (unilateral) facial pain. For initial treatment, the most narrow-spectrum agent active against the likely pathogens should be used. Herbal compounds have been commonly used in treatment of ARS, but only a few DBPC randomized studies have shown their efficacy. Hence, the benefit of herbal compounds in treatment of ARS need to be confirmed by more well designed and randomized clinical trials in future.
3.4.1. Introduction
ARS is a common disease that is managed in both primary care and specialized clinics, and by general practitioners (GPs), otolaryngologists and paediatricians. Therefore, consensus in the management of ARS amongst GPs and different specialists who commonly treat ARS is very important. However, it needs to be noticed that when analysing studies for scientific evidences in the treatment of ARS (no matter of the investigated drug) several of them present a mixture of patients with common cold and either post-viral or bacterial ARS (i.e. corticosteroids and antibiotics in ARS, Williamson IG 2007 (312)).
ARS resolves without antibiotic treatment in most cases. Symptomatic treatment and reassurance is the preferred initial management strategy for patients with mild symptoms.
It has been stated clearly in position papers and various metaanalyses that ARS resolves without antibiotic treatment in most cases (8, 293-295). Symptomatic treatment and reassurance is the preferred initial management strategy for patients with mild symptoms. Antibiotic therapy should be reserved for patients with high fever or severe (unilateral) facial pain. For initial treatment, the most narrow-spectrum agent active against the likely pathogens (Streptococcus pneumoniae and Haemophilus influenzae) should be used, rather than a general broadspectrum agent (293).
3.4.2. Treatment of ARS with antibiotics
According to data from a National Ambulatory Medical Care Survey (NAMCS) in the USA, rhinosinusitis is the fifth most common diagnosis for which an antibiotic is prescribed. In 2002, rhinosinusitis accounted for 9% and 21% of all paediatric and adult antibiotic prescriptions respectively (296), although the usage of antibiotics in the treatment of mild, moderate or uncomplicated ARS has been shown to be not useful by most randomized controlled studies (Table 3.4.1) and is not recommended by almost all clinical guidelines (8, 293-296). A recent multi-nations study in Asia showed that overuse of antibiotics is still an alarming problem among GPs, otolaryngologists, and paediatricians (9).
Summary
The introduction of evidence-based management of ARS has a major impact on the physician's management of ARS patients. It has been proven clearly in many clinical studies that ARS resolves without antibiotic treatment in most cases. Symptomatic treatment and reassurance is the preferred initial management strategy for patients with mild symptoms. Intranasal corticosteroids in monotherapy or in adjuvant therapy to oral antibiotics are proven to be effective; however, in patients with severe ARS, oral corticosteroids can be used for short-term relief of headache, facial pain and other acute symptoms. Antibiotic therapy should be reserved for patients with high fever or severe (unilateral) facial pain. For initial treatment, the most narrow-spectrum agent active against the likely pathogens should be used. Herbal compounds have been commonly used in treatment of ARS, but only a few DBPC randomized studies have shown their efficacy. Hence, the benefit of herbal compounds in treatment of ARS need to be confirmed by more well designed and randomized clinical trials in future.
3.4.1. Introduction
ARS is a common disease that is managed in both primary care and specialized clinics, and by general practitioners (GPs), otolaryngologists and paediatricians. Therefore, consensus in the management of ARS amongst GPs and different specialists who commonly treat ARS is very important. However, it needs to be noticed that when analysing studies for scientific evidences in the treatment of ARS (no matter of the investigated drug) several of them present a mixture of patients with common cold and either post-viral or bacterial ARS (i.e. corticosteroids and antibiotics in ARS, Williamson IG 2007 (312)).
ARS resolves without antibiotic treatment in most cases. Symptomatic treatment and reassurance is the preferred initial management strategy for patients with mild symptoms.
It has been stated clearly in position papers and various metaanalyses that ARS resolves without antibiotic treatment in most cases (8, 293-295). Symptomatic treatment and reassurance is the preferred initial management strategy for patients with mild symptoms. Antibiotic therapy should be reserved for patients with high fever or severe (unilateral) facial pain. For initial treatment, the most narrow-spectrum agent active against the likely pathogens (Streptococcus pneumoniae and Haemophilus influenzae) should be used, rather than a general broadspectrum agent (293).
3.4.2. Treatment of ARS with antibiotics
According to data from a National Ambulatory Medical Care Survey (NAMCS) in the USA, rhinosinusitis is the fifth most common diagnosis for which an antibiotic is prescribed. In 2002, rhinosinusitis accounted for 9% and 21% of all paediatric and adult antibiotic prescriptions respectively (296), although the usage of antibiotics in the treatment of mild, moderate or uncomplicated ARS has been shown to be not useful by most randomized controlled studies (Table 3.4.1) and is not recommended by almost all clinical guidelines (8, 293-296). A recent multi-nations study in Asia showed that overuse of antibiotics is still an alarming problem among GPs, otolaryngologists, and paediatricians (9).
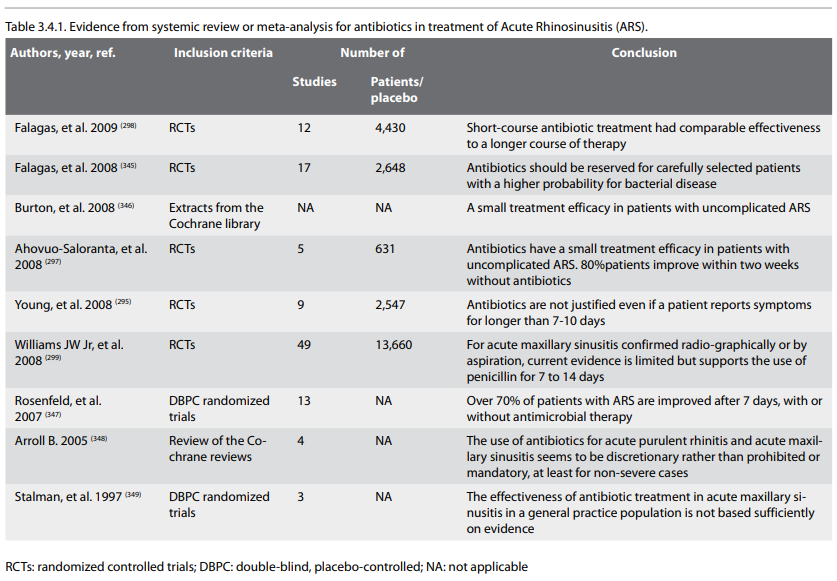
A recent Cochrane study was performed to compare antibiotics
against placebo, or between antibiotics from different classes
in the treatment of acute maxillary sinusitis in adults (297). A
total of 59 studies were included in this review; six
placebo-controlled studies and 53 studies comparing different
classes of antibiotics or comparing different dosing regimens of
the same antibiotic. Among them, 5 studies involving 631
patients provided data for comparison of antibiotics to placebo,
where clinical failure was defined as a lack of cure or
improvement at 7 to 15 days follow up. These studies found a
slight statistical difference in favour of antibiotics, compared
to placebo, with a pooled risk factor (RR) of 0.66 (95%
confidence interval (CI) 0.44 to 0.98). However, the clinical
significance of the result is equivocal, also considering that
cure or improvement rate was high in both the placebo group
(80%) and the antibiotic group (90%).
Based on six studies, where clinical failure was defined as a lack of total cure, there was significant difference in favour of antibiotics compared to placebo with a pooled RR of 0.74 (95% CI 0.65 to 0.84) at 7 to 15 days follow up. None of the antibiotic preparations was superior to another. This study concluded that antibiotics have a small treatment effect in patients with uncomplicated ARS in a primary care setting with symptoms for more than seven days. Eighty percent of patients treated without antibiotics improve within two weeks. Clinicians need to weigh the small benefits of antibiotic treatment against the potential for adverse effects at both the individual and general population level (297).
Although antibiotics for ARS should be reserved for selected patients with substantial probability of bacterial disease, accurate clinical diagnosis is often difficult to attain. Shortcourse antibiotic treatment had comparable effectiveness to a longer course of therapy for ARS. Shortened treatment, particularly for patients without severe disease and complicating factors, might lead to fewer adverse events, better patient compliance, lower rates of resistance development and fewer costs (298).
In an earlier Cochrane study (299), the authors aimed to examine whether antibiotics are indicated for ARS, and if so, which antibiotic classes are most effective. Primary outcomes were: a) clinical cure, and b) clinical cure or improvement. Secondary outcomes were radiographic improvement, relapse rates, and dropouts due to adverse effects.
A total of 49 trials, involving 13,660 participants, were evaluated with antibiotic treatment for acute maxillary sinusitis. Compared to controls (5 studies), penicillin improved clinical cures (relative risk (RR) 1.72; 95% CI 1.00 to 2.96). Treatment with amoxicillin did not significantly improve cure rates (RR 2.06; 95% CI 0.65 to 6.53) but there was significant variability between studies. Radiographic outcomes were improved by antibiotic treatment. Comparisons between classes of antibiotics (10 studies) showed no significant differences between newer non-penicillins (cephalosporins, macrolides, minocycline) versus penicillins (amoxicillin, penicillin V) with RR for cure 1.07 (95% CI 0.99 to 1.17); and newer non-penicillins versus amoxicillin-clavulanate (RR for cure 1.03; 95% CI 0.96 to 1.11). Compared to amoxicillinclavulanate (17 studies), dropouts due to adverse effects were significantly lower for cephalosporin antibiotics (RR 0.47; 95% CI 0.30 to 0.73). Relapse rates within one month of successful therapy were 7.7%. The authors conclude that, for acute maxillary sinusitis confirmed radiographically or by aspiration, current evidence is limited but supports the use of penicillin or amoxicillin for 7 to 14 days. Clinicians should weigh the moderate benefits of antibiotic treatment against the potential for adverse effects (299).
Antibiotic therapy should be reserved for patients with severe ARS, especially with the presence of high fever or severe (unilateral) facial pain. Clinicians should weigh the moderate benefits of antibiotic treatment against the potential for adverse effects.
Comparison between various antibiotics in term of their dose and duration, efficacy and side-effect of treatments are summarized in three tables, where a total of 42 prospective, randomized, double-blind, placebo controlled (n=9, Table 3.4.2), or comparisons between antibiotics (n=25, Table 3.4.3), or comparisons of different dosages (n=5) or durations (n=3) of treatment (Table 3.4.4) are listed. In general, a short-course treatment, particularly for patients without severe disease and complicating factors, might lead to fewer adverse events, better patient compliance, lower rate of resistance development and fewer costs (298).
Based on six studies, where clinical failure was defined as a lack of total cure, there was significant difference in favour of antibiotics compared to placebo with a pooled RR of 0.74 (95% CI 0.65 to 0.84) at 7 to 15 days follow up. None of the antibiotic preparations was superior to another. This study concluded that antibiotics have a small treatment effect in patients with uncomplicated ARS in a primary care setting with symptoms for more than seven days. Eighty percent of patients treated without antibiotics improve within two weeks. Clinicians need to weigh the small benefits of antibiotic treatment against the potential for adverse effects at both the individual and general population level (297).
Although antibiotics for ARS should be reserved for selected patients with substantial probability of bacterial disease, accurate clinical diagnosis is often difficult to attain. Shortcourse antibiotic treatment had comparable effectiveness to a longer course of therapy for ARS. Shortened treatment, particularly for patients without severe disease and complicating factors, might lead to fewer adverse events, better patient compliance, lower rates of resistance development and fewer costs (298).
In an earlier Cochrane study (299), the authors aimed to examine whether antibiotics are indicated for ARS, and if so, which antibiotic classes are most effective. Primary outcomes were: a) clinical cure, and b) clinical cure or improvement. Secondary outcomes were radiographic improvement, relapse rates, and dropouts due to adverse effects.
A total of 49 trials, involving 13,660 participants, were evaluated with antibiotic treatment for acute maxillary sinusitis. Compared to controls (5 studies), penicillin improved clinical cures (relative risk (RR) 1.72; 95% CI 1.00 to 2.96). Treatment with amoxicillin did not significantly improve cure rates (RR 2.06; 95% CI 0.65 to 6.53) but there was significant variability between studies. Radiographic outcomes were improved by antibiotic treatment. Comparisons between classes of antibiotics (10 studies) showed no significant differences between newer non-penicillins (cephalosporins, macrolides, minocycline) versus penicillins (amoxicillin, penicillin V) with RR for cure 1.07 (95% CI 0.99 to 1.17); and newer non-penicillins versus amoxicillin-clavulanate (RR for cure 1.03; 95% CI 0.96 to 1.11). Compared to amoxicillinclavulanate (17 studies), dropouts due to adverse effects were significantly lower for cephalosporin antibiotics (RR 0.47; 95% CI 0.30 to 0.73). Relapse rates within one month of successful therapy were 7.7%. The authors conclude that, for acute maxillary sinusitis confirmed radiographically or by aspiration, current evidence is limited but supports the use of penicillin or amoxicillin for 7 to 14 days. Clinicians should weigh the moderate benefits of antibiotic treatment against the potential for adverse effects (299).
Antibiotic therapy should be reserved for patients with severe ARS, especially with the presence of high fever or severe (unilateral) facial pain. Clinicians should weigh the moderate benefits of antibiotic treatment against the potential for adverse effects.
Comparison between various antibiotics in term of their dose and duration, efficacy and side-effect of treatments are summarized in three tables, where a total of 42 prospective, randomized, double-blind, placebo controlled (n=9, Table 3.4.2), or comparisons between antibiotics (n=25, Table 3.4.3), or comparisons of different dosages (n=5) or durations (n=3) of treatment (Table 3.4.4) are listed. In general, a short-course treatment, particularly for patients without severe disease and complicating factors, might lead to fewer adverse events, better patient compliance, lower rate of resistance development and fewer costs (298).
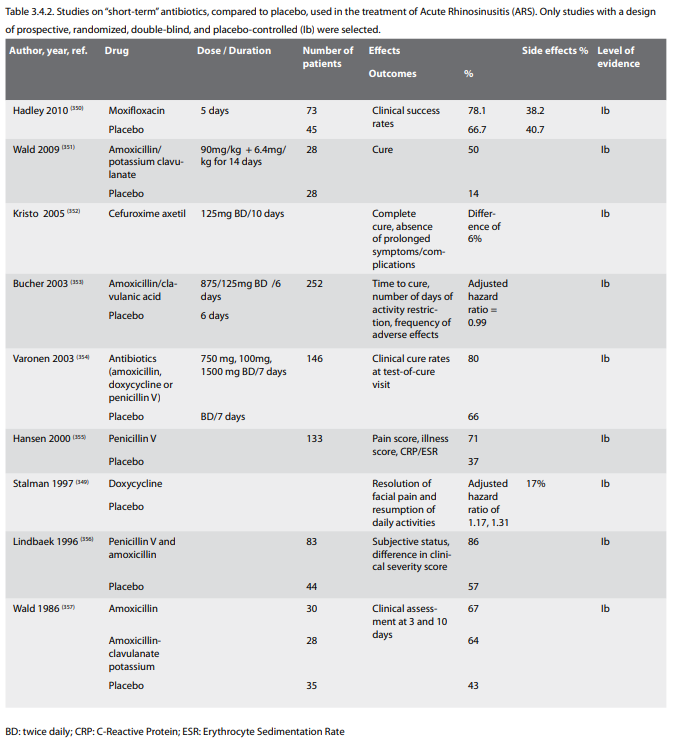
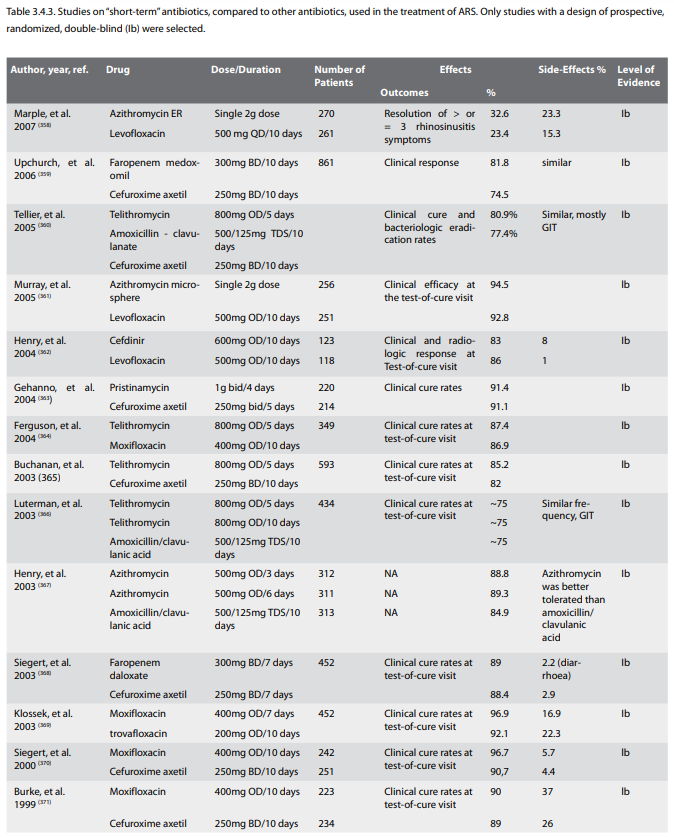
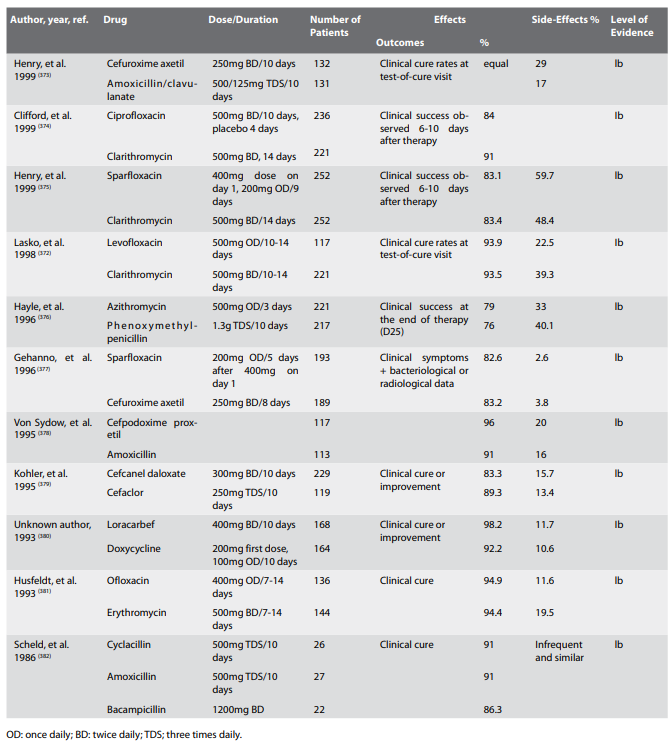
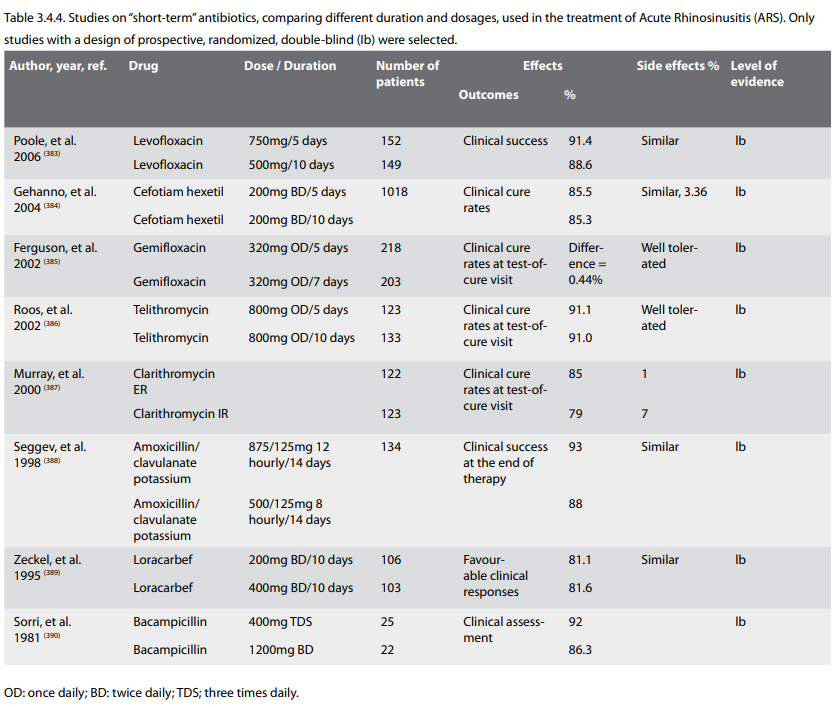
Antibiotics overuse has been reported in some European countries
(300, 301) to have directly resulted in an increased prevalence
of antimicrobial resistance in Europe (302, 303).
Although such data is still unavailable in Asia, a recent survey study showed that, even for mild ARS (common cold), medical treatments were still recommended by 87% of GPs, 83.9% of otolaryngologists, and 70% of paediatricians (9). The top three first-line treatments prescribed were antihistamines (39.2%), nasal decongestants (33.6%), and antibiotics (29.5%). Antibiotics usage was much more often used as the first line treatment of moderate (45.9%) and severe (60.3%) ARS. Even more alarmingly, 13.6% of the participants used a combination of more than two antibiotics classes for treatment of even mild ARS.
The global threat posed by resistant microorganisms has become an international health issue, a product of careless antibiotics abuse. Therefore, for initial treatment, the most narrow-spectrum agent active against the likely pathogens (Streptococcus pneumoniae and Haemophilus influenzae) should be used (293).
3.4.3. Treatment with intranasal corticosteroids
3.4.3.1. Treatment with intranasal corticosteroids
In the EP3 OS 2007 document, intranasal corticosteroids were recommended for the treatment of ARS, both in moderate (monotherapy) and severe (with oral antibiotics) disease.
Intranasal corticosteroids are recommended for the treatment of ARS, both in moderate (monotherapy) and severe (with oral antibiotics) disease.
Most studies on corticosteroids in ARS have determined the effect of topical corticosteroids when used as adjunct therapy to antibiotics (Table 3.4.5) (304-309). Recently a double-blind, doubledummy, placebo-controlled study was published in which topical corticosteroid treatment was used as monotherapy and compared to antibiotics (310). In this study mometasone furoate (MF) was used and compared to both amoxicillin and placebo in ARS. MF 200 µg twice daily was significantly superior to placebo and amoxicillin in improving the symptom score. Used once daily MF was also superior to placebo but not to amoxicillin. This is the first study to show that topical corticosteroids when used twice daily are effective in treating ARS as monotherapy and is more effective than amoxicillin when used twice daily. Data of this study are also supported by two other studies with a similar design (Table 3.4.5) (311,1367). However, in another study, neither antibiotics nor topical corticosteroids alone or in combination were effective in altering the symptom severity or the duration of bacterial ARS (312). However, this study has included patients with 4 days of symptoms, which only satisfy the inclusion criteria of common cold but not ARS.
Although such data is still unavailable in Asia, a recent survey study showed that, even for mild ARS (common cold), medical treatments were still recommended by 87% of GPs, 83.9% of otolaryngologists, and 70% of paediatricians (9). The top three first-line treatments prescribed were antihistamines (39.2%), nasal decongestants (33.6%), and antibiotics (29.5%). Antibiotics usage was much more often used as the first line treatment of moderate (45.9%) and severe (60.3%) ARS. Even more alarmingly, 13.6% of the participants used a combination of more than two antibiotics classes for treatment of even mild ARS.
The global threat posed by resistant microorganisms has become an international health issue, a product of careless antibiotics abuse. Therefore, for initial treatment, the most narrow-spectrum agent active against the likely pathogens (Streptococcus pneumoniae and Haemophilus influenzae) should be used (293).
3.4.3. Treatment with intranasal corticosteroids
3.4.3.1. Treatment with intranasal corticosteroids
In the EP3 OS 2007 document, intranasal corticosteroids were recommended for the treatment of ARS, both in moderate (monotherapy) and severe (with oral antibiotics) disease.
Intranasal corticosteroids are recommended for the treatment of ARS, both in moderate (monotherapy) and severe (with oral antibiotics) disease.
Most studies on corticosteroids in ARS have determined the effect of topical corticosteroids when used as adjunct therapy to antibiotics (Table 3.4.5) (304-309). Recently a double-blind, doubledummy, placebo-controlled study was published in which topical corticosteroid treatment was used as monotherapy and compared to antibiotics (310). In this study mometasone furoate (MF) was used and compared to both amoxicillin and placebo in ARS. MF 200 µg twice daily was significantly superior to placebo and amoxicillin in improving the symptom score. Used once daily MF was also superior to placebo but not to amoxicillin. This is the first study to show that topical corticosteroids when used twice daily are effective in treating ARS as monotherapy and is more effective than amoxicillin when used twice daily. Data of this study are also supported by two other studies with a similar design (Table 3.4.5) (311,1367). However, in another study, neither antibiotics nor topical corticosteroids alone or in combination were effective in altering the symptom severity or the duration of bacterial ARS (312). However, this study has included patients with 4 days of symptoms, which only satisfy the inclusion criteria of common cold but not ARS.
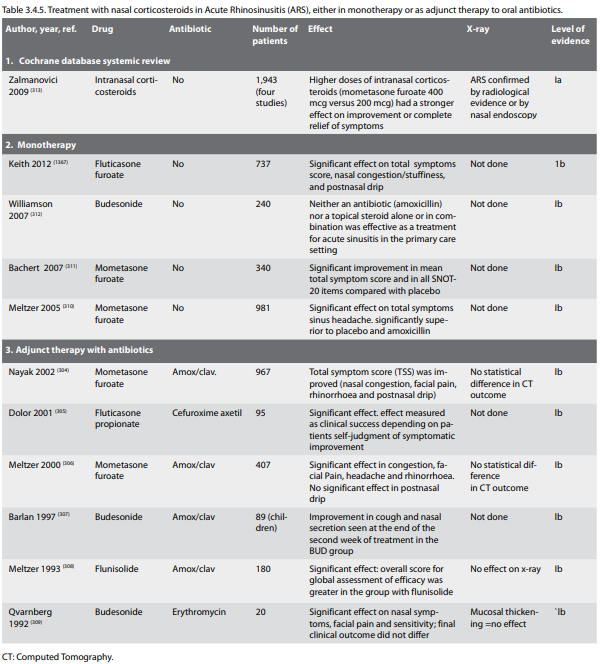
In a recent Cochrane analysis, the results of four DBPC studies
with a total of 1945 patients support the use of intranasal
corticosteroids as a monotherapy or as an adjuvant therapy to
antibiotics (evidence level Ia) (313). Higher doses of
intranasal corticosteroids had a stronger effect on improvement
or complete relief of symptoms; for mometasone furoate 400 µg
versus 200 µg, (RR 1.10; 95% CI 1.02 to 1.18 versus RR 1.04; 95%
CI 0.98 to 1.11). No significant adverse events were reported
and there was no significant difference in the drop-out and
recurrence rate for the two treatment groups and for groups
receiving higher doses of intranasal corticosteroids. In the
future, further randomized clinical studies are needed to study
the efficacy and appropriate use of antibiotics and intranasal
corticosteroids as mono- or combined therapy in the treatment of
ARS with different severities.
3.4.3.2. Oral corticosteroids adjunct therapy
The result of a recent Cochrane analysis suggests that oral corticosteroids as an adjunctive therapy to oral antibiotics are effective for short-term relief of symptoms (e.g., headache, facial pain, nasal decongestion and etc.) in ARS (evidence level Ia) (314).
Gehanno et al. (315) tried 8 mg methylprednisolone three times daily for 5 days as adjunctive therapy to 10 days treatment with amoxicillin clavulanate potassium in patients with ARS (criteria: symptoms < 10 days, craniofacial pain, purulent nasal discharge with purulent drainage from the middle meatus, opacities of the sinuses in x-ray or CT scan) in a placebo controlled study. No difference was seen in therapeutic outcome at day 14 between the groups (n=417) but at day 4 there was a significant reduction of headache and facial pain in the steroid group (Table 3.4.6). In a multicentre study Klossek et al. (316) assessed in a double blind, randomised study in parallel groups the efficacy and tolerance to prednisone administered for 3 days in addition to cefpodoxime in adult patients presenting with an ABRS (proven by culture) with severe pain. The assessments made during the first 3 days of treatment showed a statistically significant difference in favour of the prednisone group regarding pain, nasal obstruction and consumption of paracetamol (Table 3.4.6). There was no difference between the two groups after the end of the antibiotic treatment. The tolerance measured throughout the study was comparable between the two groups. Pain is significantly relieved during treatment with prednisone but after 10 days on antibiotics there was no difference between the two groups.
The long-term use of systemic steroids bears the wellrecognized risk of these drugs. Since evidence on the use of corticosteroids in patients with ARS is scarce, high-quality trials assessing the efficacy of systemic corticosteroids both as an adjuvant and a monotherapy in the primary care setting should be initiated to provide a more definite answer on their use. These trials should report both short-term (< two weeks) and long-term (> two weeks) effects as well as information on relapse rates and adverse events (314).
3.4.3.3. Prophylactic treatment of recurrent episodes
In a study by Puhakka et al. (317), fluticasone propionate (FP, 200 μg four times daily) or placebo were used for 6 days in 199 subjects with an acute common cold, 24-48 hours after onset of symptoms, to study the preventive effects of FP on risk for development of ARS. Frequency of sinusitis at day 7 in subjects with a positive culture of rhinovirus in nasopharyngeal aspirates, based on x-ray, was 18.4% and 34.9% in FP and placebo group respectively (p=0.07) thus indicating a non-significant effect of FP. Indeed, there is very low evidence for a prophylactic effect of nasal corticosteroids in prevention of recurrence of ARS episodes.
3.4.4. Other treatments
A large number of trials and Cochrane reviews are performed in viral rhinosinusitis. In general the studies are of low quality making clear recommendations difficult.
3.4.4.1. Oral antihistamines
There is no indication for the use of antihistamines (both intranasal and oral) in the treatment of post viral ARS, except in co-existing allergic rhinitis.
Oral antihistamines are frequently prescribed drugs especially for mild ARS (9). Antihistamines are standard treatment for IgE-mediated allergic diseases such as allergic rhinitis, where histamine (released by mast cells and basophils) is one of the major effectors of allergic reaction (318, 319). The pathophysiology of ARS is felt to be secondary bacterial infection due to the impairment of mechanical, humoral and cellular defences and epithelial damage caused by viral infection (common cold) (8). Antihistamines may be marginally more effective at reducing symptoms of runny nose and sneezing at 2 days in viral rhinosinusitis (1365). There is no indication for the use of antihistamines (both intranasal and oral) in the treatment of postviral ARS, except in co-existing allergic rhinitis.
3.4.4.2. Nasal decongestants
Nasal decongestants are commonly applied in the treatment of ARS in order to decrease congestion and in the hope of improving better sinus ventilation and drainage, as well as to provide symptomatic relief of nasal congestion. Experimental trials on the effect of topical decongestants by CT (320) and MRI scans (321) on ostial and ostiomeatal complex patency have confirmed marked effect on reducing congestion of inferior and middle turbinates and infundibular mucosa, but no effect on ethmoidal and maxillary sinus mucosa. Experimental studies suggest beneficial anti-inflammatory effect of xylometazoline and oxymetazoline by decreasing nitric oxide synthetase (322) and their anti-oxidant action (323).
In contrast to previous in vitro trials on the effect of decongestants on mucociliary transport, a controlled clinical trial (evidence level II) by Inanli et al. suggested improvement in mucociliary clearance in vivo, after 2 weeks of oxymetazoline application in acute bacterial rhinosinusitis, compared to fluticasone, hypertonic saline and saline, but it did not show significant improvement compared to the group where no topical nasal treatment was given. Also, the clinical course of the disease between the groups was not significantly different (324). This is in concordance with previous randomized controlled trial in adult acute maxillary sinusitis (evidence level Ib), which did not prove any significant impact of decongestants when added to a penicillin treatment regime in terms of daily symptoms scores of headache and obstruction and sinus x-ray scores (325). Therefore, the results of this study suggest that decongestion of the sinus ostia is not of primary importance during the course of healing of ARS.
A single dose of a decongestant (oral norephedrine, topical oxymetazoline, oral pseudoephedrine, nasal xylometazoline may be marginally more effective than placebo at reducing congestion at 3 to 10 hours in patients with viral rhinosinusitis(1365). Decongestant treatment did not prove superior to saline, when added to antibiotic and antihistamine treatment in a randomized double-blind placebo-controlled trial for acute paediatric rhinosinusitis (evidence level Ib) (326). However, a double blind, randomized, placebo controlled trial demonstrated a significant protective effect of a 14-day course of nasal decongestant (combined with topical budesonide after 7 days) in the prevention of the development of nosocomial maxillary sinusitis in mechanically ventilated patients in the intensive care unit. (327). Radiologically confirmed maxillary sinusitis was observed in 54% of patients in the active treatment group and in the 82% of the controls, respectively, while infective maxillary sinusitis was observed in 8% and 20% of the groups, respectively (327). Clinical experience, however, supports the use of the topical application of decongestants to the middle meatus in ARS but not by nasal spray or nasal drops (Evidence level IV).
Recently, a systematically review (Cochrane analysis) of the efficacy of decongestants, antihistamines and nasal irrigation in children with clinically diagnosed ARS was reported (328). Of the 402 studies found through the electronic searches and handsearching, none met all the inclusion criteria (any one of these drugs versus placebo or no medication). It concludes that no evidence to determine whether the use of antihistamines, decongestants or nasal irrigation is efficacious in children with ARS.
In another Cochrane review the effectiveness of antihistaminedecongestant-analgesic combinations in reducing the duration and alleviating the symptoms of the common cold in adults and children was assessed. The authors included 27 trials (5117 participants) of randomised controlled trials investigating the effectiveness of common cold treatments. Fourteen trials studied antihistamine-decongestant combinations. The authors conclude that current evidence suggests that antihistamineanalgesic-decongestant combinations have some general benefit in adults and older children (recommendation A). They recommend to weighed the benefits against the risk of adverse effects. They found is no evidence of effectiveness in young children (1363).
3.4.4.3. Nasal or antral irrigation
Nasal irrigation with saline solution has a limited effect in adults with ARS.
Nasal irrigation is a procedure that rinses the nasal cavity with water, isotonic or hypertonic saline solutions. Other synonyms have also been used in the literature such as nasal douche, wash, or lavage. A number of randomized controlled trials have tested nasal and antral irrigation with isotonic or hypertonic saline in the treatment of ARS and CRS. Although saline is considered as a control treatment itself, patients in these randomized trials were assigned to different modalities of application of saline or hypertonic saline, or hypertonic compared to isotonic saline. The results between the groups were compared. Most of them offer evidence that nasal washouts or irrigations with isotonic or hypertonic saline are beneficial in terms of alleviation of symptoms. Hypertonic saline is preferred to isotonic saline in the treatment of rhinosinusitis by some authors in the USA, mostly based on a paper indicating that it significantly improves nasal mucociliary clearance measured by saccharine testing in healthy volunteers (329).
A randomized trial (Ib) by Adam et al. (330) with two controls compared hypertonic nasal saline to isotonic saline and no treatment in 119 patients with common cold and ARS (which were the majority). Outcome measures were subjective nasal symptoms scores (congestion, secretion, headache) at day-3, day-8/-10 and the day of symptom resolution. Rhinosinusitis patients (98%) were also treated with antibiotics. There was no difference between the groups and only 44% of the patients would use the hypertonic saline spray again. Thirty-two percent noted burning, compared with 13% of the normal saline group.
Antral irrigation did not offer significant benefit when added to standard 10-day antibiotic treatment in (4 antibiotics+ decongestants vs. antral washouts; 50 patients per group) ARS, demonstrating approximately 5% better cure rate in each group for washouts than for decongestants, which was not significant (331).
More recently, a review of the Cochrane data from randomised controlled trials (3 RCTs with 618 participants) comparing topical nasal saline treatment to other interventions in adults and children with clinically diagnosed acute URTIs (common cold and rhinosinusitis) has been reported. Most results showed no difference between nasal saline treatment and control. However, there was limited evidence of benefit with nasal saline irrigation in adults. One study showed a mean difference of 0.3 day (out of eight days) for symptom resolution, but this was not significant. Nasal saline irrigation was associated with less time off work in one study. Minor discomfort was not uncommon and 40% of babies did not tolerate nasal saline drops (332).
Another systematic review of literature was performed to determine whether nasal douching is effective in the treatment of ARS and in preventing recurrent upper respiratory tract infections. The results showed that nasal douching with saline solution has a limited effect in adults with ARS (level of evidence Ia). It is effective in children with ARS in addition to the standard medication (level of evidence Ib) and can prevent recurrent infections (level of evidence IIb) (333).
3.4.4.4. Heated, humidified air
Heated, humidified air has long been used by sufferers of the common cold. The theoretical basis is that steam may help congested mucus drain better and heat may destroy the cold virus as it does in vitro. Six trials (394 trial participants) were included. Three trials in which patient data could be pooled found benefits of steam for symptom relief for the common cold (odds ratio (OR) 0.31; 95% confidence interval (CI) 0.16 to 0.60). However, results on symptom indices were equivocal. In conclusion steam inhalation has not shown any consistent benefits in the treatment of the common cold, hence is not recommended in the routine treatment of common cold symptoms until more double-blind, randomized trials with a standardised treatment modality are conducted (recommendation A(-)) (1364).
3.4.4.5. Physical interventions to interrupt or reduce the spread of respiratory viruses in viral rhinosinusitis
A cochrane review was performed to systematically review the effectiveness of physical interventions to interrupt or reduce the spread of respiratory viruses. The randomized studies suggest respiratory virus spread can be prevented by hygienic measures, such as handwashing, especially around younger children. The incremental effect of adding virucidals or antiseptics to normal handwashing to decrease respiratory disease remains uncertain. Case-control studies suggested that implementing barriers to transmission, isolation, and hygienic measures are effective at containing respiratory virus epidemics. There was limited evidence that social distancing was effective especially if related to the risk of exposure (recommendation A)(1358).
3.4.4.6. Ipratropium bromide
A Cochrane review was performed to determine the effect of ipratropium bromide versus placebo or no treatment on severity of rhinorrhoea and nasal congestion in children and adults with the common cold. Seven trials (2144 participants). Four studies (1959 participants) addressed subjective change in severity of rhinorrhoea. All studies were consistent in reporting statistically significant changes in favour of IB. Nasal congestion was reported in four studies and was found to have no significant change between the two groups. The authors conclude that for people with common cold, the existing evidence, which has some limitations, suggests that Ipratropium bromide is likely to be effective in ameliorating rhinorrhoea. Ipratropium bromide had no effect on nasal congestion and its use was associated with more side effects compared to placebo or no treatment although these appeared to be well-tolerated and self-limiting (recommendation A)(1361).
3.4.4.7. Probiotics
A Cochrane review was performed to assess the effectiveness and safety of probiotics for preventing acute URTIs. The authors included 14 RCTs, but only available data to meta-analyse could be extracted from 10 trials (3451 participants). Probiotics were better than placebo in reducing the number of participants experiencing episodes of acute URTIs, the rate ratio of episodes of acute URTI and reducing antibiotic use (recommendation A) (1362).
3.4.4.8. Vaccination
Vaccination has no direct effect in treatment of ARS. However, routine childhood vaccination has affected frequency and bacteriology of acute otitis media (AOM) and acute bacterial rhinosinusitis (341). It was found that immunization leads to increase of host's resistance capabilities, decrease of acute respiratory disease incidence and changes in structure of complications due to infection (342). In another study, a significant shift occurred in the causative pathogens of acute maxillary sinusitis in children in the 5 years after the introduction of vaccination of children with the 7-valent pneumococcal vaccine (PCV7) as compared to the previous 5 years. While the proportion of S. pneumoniae declined by 18%, the proportion of H. influenzae increased by 8% (108).
3.4.4.9. NSAID's, Aspirin or acetominophen
In a multicentre, randomized, double-blind, double-dummy, placebo-controlled study, 392 patients with URTI received a single dose of aspirin 500 or 1,000 mg, acetaminophen 500 or 1,000 mg, or matching placebo (343). Significant reductions were seen in the mean intensity of headache, achiness, and feverish discomfort with all active treatments (P < 0.001), but not in sinus sensitivity to percussion or sore throat (evidence level Ib). A Cochrane review was performed to determine the effects and adverse effects of NSAID's versus placebo and other treatments on the signs and symptoms of the common cold. The review included nine RCTs, describing 37 comparisons: six were NSAID's versus placebo, and three were NSAID's versus NSAID's (1064 patients with common cold). NSAID's did not significantly reduce the total symptom score, or duration of colds. However, for outcomes related to the analgesic effects of NSAID's (headache, ear pain, and muscle and joint pain) NSAID's produced significant benefits. There was no evidence of increased frequency of adverse effects in the NSAID's treatment groups. The authors recommend NSAID's for relieving discomfort or pain caused by the common cold (1357).
3.4.4.10. Zinc
The Cochrane review Zinc and the common cold included 15 randomized controlled double-blind trials. It was concluded, that zinc would shorten the duration of the episode of common cold and also could be used as a prevention so that the risk of developing an episode of common cold would be decreased. It is too early to give general recommendations for the use of zinc as we do not have sufficient knowledge about the optimal dose, formulation and duration of treatment. Further research should focus on the effect of zinc in patients who are at increased risk of developing complications after common cold (recommendation C) (1352,1356).
3.4.3.2. Oral corticosteroids adjunct therapy
The result of a recent Cochrane analysis suggests that oral corticosteroids as an adjunctive therapy to oral antibiotics are effective for short-term relief of symptoms (e.g., headache, facial pain, nasal decongestion and etc.) in ARS (evidence level Ia) (314).
Gehanno et al. (315) tried 8 mg methylprednisolone three times daily for 5 days as adjunctive therapy to 10 days treatment with amoxicillin clavulanate potassium in patients with ARS (criteria: symptoms < 10 days, craniofacial pain, purulent nasal discharge with purulent drainage from the middle meatus, opacities of the sinuses in x-ray or CT scan) in a placebo controlled study. No difference was seen in therapeutic outcome at day 14 between the groups (n=417) but at day 4 there was a significant reduction of headache and facial pain in the steroid group (Table 3.4.6). In a multicentre study Klossek et al. (316) assessed in a double blind, randomised study in parallel groups the efficacy and tolerance to prednisone administered for 3 days in addition to cefpodoxime in adult patients presenting with an ABRS (proven by culture) with severe pain. The assessments made during the first 3 days of treatment showed a statistically significant difference in favour of the prednisone group regarding pain, nasal obstruction and consumption of paracetamol (Table 3.4.6). There was no difference between the two groups after the end of the antibiotic treatment. The tolerance measured throughout the study was comparable between the two groups. Pain is significantly relieved during treatment with prednisone but after 10 days on antibiotics there was no difference between the two groups.
The long-term use of systemic steroids bears the wellrecognized risk of these drugs. Since evidence on the use of corticosteroids in patients with ARS is scarce, high-quality trials assessing the efficacy of systemic corticosteroids both as an adjuvant and a monotherapy in the primary care setting should be initiated to provide a more definite answer on their use. These trials should report both short-term (< two weeks) and long-term (> two weeks) effects as well as information on relapse rates and adverse events (314).
3.4.3.3. Prophylactic treatment of recurrent episodes
In a study by Puhakka et al. (317), fluticasone propionate (FP, 200 μg four times daily) or placebo were used for 6 days in 199 subjects with an acute common cold, 24-48 hours after onset of symptoms, to study the preventive effects of FP on risk for development of ARS. Frequency of sinusitis at day 7 in subjects with a positive culture of rhinovirus in nasopharyngeal aspirates, based on x-ray, was 18.4% and 34.9% in FP and placebo group respectively (p=0.07) thus indicating a non-significant effect of FP. Indeed, there is very low evidence for a prophylactic effect of nasal corticosteroids in prevention of recurrence of ARS episodes.
3.4.4. Other treatments
A large number of trials and Cochrane reviews are performed in viral rhinosinusitis. In general the studies are of low quality making clear recommendations difficult.
3.4.4.1. Oral antihistamines
There is no indication for the use of antihistamines (both intranasal and oral) in the treatment of post viral ARS, except in co-existing allergic rhinitis.
Oral antihistamines are frequently prescribed drugs especially for mild ARS (9). Antihistamines are standard treatment for IgE-mediated allergic diseases such as allergic rhinitis, where histamine (released by mast cells and basophils) is one of the major effectors of allergic reaction (318, 319). The pathophysiology of ARS is felt to be secondary bacterial infection due to the impairment of mechanical, humoral and cellular defences and epithelial damage caused by viral infection (common cold) (8). Antihistamines may be marginally more effective at reducing symptoms of runny nose and sneezing at 2 days in viral rhinosinusitis (1365). There is no indication for the use of antihistamines (both intranasal and oral) in the treatment of postviral ARS, except in co-existing allergic rhinitis.
3.4.4.2. Nasal decongestants
Nasal decongestants are commonly applied in the treatment of ARS in order to decrease congestion and in the hope of improving better sinus ventilation and drainage, as well as to provide symptomatic relief of nasal congestion. Experimental trials on the effect of topical decongestants by CT (320) and MRI scans (321) on ostial and ostiomeatal complex patency have confirmed marked effect on reducing congestion of inferior and middle turbinates and infundibular mucosa, but no effect on ethmoidal and maxillary sinus mucosa. Experimental studies suggest beneficial anti-inflammatory effect of xylometazoline and oxymetazoline by decreasing nitric oxide synthetase (322) and their anti-oxidant action (323).
In contrast to previous in vitro trials on the effect of decongestants on mucociliary transport, a controlled clinical trial (evidence level II) by Inanli et al. suggested improvement in mucociliary clearance in vivo, after 2 weeks of oxymetazoline application in acute bacterial rhinosinusitis, compared to fluticasone, hypertonic saline and saline, but it did not show significant improvement compared to the group where no topical nasal treatment was given. Also, the clinical course of the disease between the groups was not significantly different (324). This is in concordance with previous randomized controlled trial in adult acute maxillary sinusitis (evidence level Ib), which did not prove any significant impact of decongestants when added to a penicillin treatment regime in terms of daily symptoms scores of headache and obstruction and sinus x-ray scores (325). Therefore, the results of this study suggest that decongestion of the sinus ostia is not of primary importance during the course of healing of ARS.
A single dose of a decongestant (oral norephedrine, topical oxymetazoline, oral pseudoephedrine, nasal xylometazoline may be marginally more effective than placebo at reducing congestion at 3 to 10 hours in patients with viral rhinosinusitis(1365). Decongestant treatment did not prove superior to saline, when added to antibiotic and antihistamine treatment in a randomized double-blind placebo-controlled trial for acute paediatric rhinosinusitis (evidence level Ib) (326). However, a double blind, randomized, placebo controlled trial demonstrated a significant protective effect of a 14-day course of nasal decongestant (combined with topical budesonide after 7 days) in the prevention of the development of nosocomial maxillary sinusitis in mechanically ventilated patients in the intensive care unit. (327). Radiologically confirmed maxillary sinusitis was observed in 54% of patients in the active treatment group and in the 82% of the controls, respectively, while infective maxillary sinusitis was observed in 8% and 20% of the groups, respectively (327). Clinical experience, however, supports the use of the topical application of decongestants to the middle meatus in ARS but not by nasal spray or nasal drops (Evidence level IV).
Recently, a systematically review (Cochrane analysis) of the efficacy of decongestants, antihistamines and nasal irrigation in children with clinically diagnosed ARS was reported (328). Of the 402 studies found through the electronic searches and handsearching, none met all the inclusion criteria (any one of these drugs versus placebo or no medication). It concludes that no evidence to determine whether the use of antihistamines, decongestants or nasal irrigation is efficacious in children with ARS.
In another Cochrane review the effectiveness of antihistaminedecongestant-analgesic combinations in reducing the duration and alleviating the symptoms of the common cold in adults and children was assessed. The authors included 27 trials (5117 participants) of randomised controlled trials investigating the effectiveness of common cold treatments. Fourteen trials studied antihistamine-decongestant combinations. The authors conclude that current evidence suggests that antihistamineanalgesic-decongestant combinations have some general benefit in adults and older children (recommendation A). They recommend to weighed the benefits against the risk of adverse effects. They found is no evidence of effectiveness in young children (1363).
3.4.4.3. Nasal or antral irrigation
Nasal irrigation with saline solution has a limited effect in adults with ARS.
Nasal irrigation is a procedure that rinses the nasal cavity with water, isotonic or hypertonic saline solutions. Other synonyms have also been used in the literature such as nasal douche, wash, or lavage. A number of randomized controlled trials have tested nasal and antral irrigation with isotonic or hypertonic saline in the treatment of ARS and CRS. Although saline is considered as a control treatment itself, patients in these randomized trials were assigned to different modalities of application of saline or hypertonic saline, or hypertonic compared to isotonic saline. The results between the groups were compared. Most of them offer evidence that nasal washouts or irrigations with isotonic or hypertonic saline are beneficial in terms of alleviation of symptoms. Hypertonic saline is preferred to isotonic saline in the treatment of rhinosinusitis by some authors in the USA, mostly based on a paper indicating that it significantly improves nasal mucociliary clearance measured by saccharine testing in healthy volunteers (329).
A randomized trial (Ib) by Adam et al. (330) with two controls compared hypertonic nasal saline to isotonic saline and no treatment in 119 patients with common cold and ARS (which were the majority). Outcome measures were subjective nasal symptoms scores (congestion, secretion, headache) at day-3, day-8/-10 and the day of symptom resolution. Rhinosinusitis patients (98%) were also treated with antibiotics. There was no difference between the groups and only 44% of the patients would use the hypertonic saline spray again. Thirty-two percent noted burning, compared with 13% of the normal saline group.
Antral irrigation did not offer significant benefit when added to standard 10-day antibiotic treatment in (4 antibiotics+ decongestants vs. antral washouts; 50 patients per group) ARS, demonstrating approximately 5% better cure rate in each group for washouts than for decongestants, which was not significant (331).
More recently, a review of the Cochrane data from randomised controlled trials (3 RCTs with 618 participants) comparing topical nasal saline treatment to other interventions in adults and children with clinically diagnosed acute URTIs (common cold and rhinosinusitis) has been reported. Most results showed no difference between nasal saline treatment and control. However, there was limited evidence of benefit with nasal saline irrigation in adults. One study showed a mean difference of 0.3 day (out of eight days) for symptom resolution, but this was not significant. Nasal saline irrigation was associated with less time off work in one study. Minor discomfort was not uncommon and 40% of babies did not tolerate nasal saline drops (332).
Another systematic review of literature was performed to determine whether nasal douching is effective in the treatment of ARS and in preventing recurrent upper respiratory tract infections. The results showed that nasal douching with saline solution has a limited effect in adults with ARS (level of evidence Ia). It is effective in children with ARS in addition to the standard medication (level of evidence Ib) and can prevent recurrent infections (level of evidence IIb) (333).
3.4.4.4. Heated, humidified air
Heated, humidified air has long been used by sufferers of the common cold. The theoretical basis is that steam may help congested mucus drain better and heat may destroy the cold virus as it does in vitro. Six trials (394 trial participants) were included. Three trials in which patient data could be pooled found benefits of steam for symptom relief for the common cold (odds ratio (OR) 0.31; 95% confidence interval (CI) 0.16 to 0.60). However, results on symptom indices were equivocal. In conclusion steam inhalation has not shown any consistent benefits in the treatment of the common cold, hence is not recommended in the routine treatment of common cold symptoms until more double-blind, randomized trials with a standardised treatment modality are conducted (recommendation A(-)) (1364).
3.4.4.5. Physical interventions to interrupt or reduce the spread of respiratory viruses in viral rhinosinusitis
A cochrane review was performed to systematically review the effectiveness of physical interventions to interrupt or reduce the spread of respiratory viruses. The randomized studies suggest respiratory virus spread can be prevented by hygienic measures, such as handwashing, especially around younger children. The incremental effect of adding virucidals or antiseptics to normal handwashing to decrease respiratory disease remains uncertain. Case-control studies suggested that implementing barriers to transmission, isolation, and hygienic measures are effective at containing respiratory virus epidemics. There was limited evidence that social distancing was effective especially if related to the risk of exposure (recommendation A)(1358).
3.4.4.6. Ipratropium bromide
A Cochrane review was performed to determine the effect of ipratropium bromide versus placebo or no treatment on severity of rhinorrhoea and nasal congestion in children and adults with the common cold. Seven trials (2144 participants). Four studies (1959 participants) addressed subjective change in severity of rhinorrhoea. All studies were consistent in reporting statistically significant changes in favour of IB. Nasal congestion was reported in four studies and was found to have no significant change between the two groups. The authors conclude that for people with common cold, the existing evidence, which has some limitations, suggests that Ipratropium bromide is likely to be effective in ameliorating rhinorrhoea. Ipratropium bromide had no effect on nasal congestion and its use was associated with more side effects compared to placebo or no treatment although these appeared to be well-tolerated and self-limiting (recommendation A)(1361).
3.4.4.7. Probiotics
A Cochrane review was performed to assess the effectiveness and safety of probiotics for preventing acute URTIs. The authors included 14 RCTs, but only available data to meta-analyse could be extracted from 10 trials (3451 participants). Probiotics were better than placebo in reducing the number of participants experiencing episodes of acute URTIs, the rate ratio of episodes of acute URTI and reducing antibiotic use (recommendation A) (1362).
3.4.4.8. Vaccination
Vaccination has no direct effect in treatment of ARS. However, routine childhood vaccination has affected frequency and bacteriology of acute otitis media (AOM) and acute bacterial rhinosinusitis (341). It was found that immunization leads to increase of host's resistance capabilities, decrease of acute respiratory disease incidence and changes in structure of complications due to infection (342). In another study, a significant shift occurred in the causative pathogens of acute maxillary sinusitis in children in the 5 years after the introduction of vaccination of children with the 7-valent pneumococcal vaccine (PCV7) as compared to the previous 5 years. While the proportion of S. pneumoniae declined by 18%, the proportion of H. influenzae increased by 8% (108).
3.4.4.9. NSAID's, Aspirin or acetominophen
In a multicentre, randomized, double-blind, double-dummy, placebo-controlled study, 392 patients with URTI received a single dose of aspirin 500 or 1,000 mg, acetaminophen 500 or 1,000 mg, or matching placebo (343). Significant reductions were seen in the mean intensity of headache, achiness, and feverish discomfort with all active treatments (P < 0.001), but not in sinus sensitivity to percussion or sore throat (evidence level Ib). A Cochrane review was performed to determine the effects and adverse effects of NSAID's versus placebo and other treatments on the signs and symptoms of the common cold. The review included nine RCTs, describing 37 comparisons: six were NSAID's versus placebo, and three were NSAID's versus NSAID's (1064 patients with common cold). NSAID's did not significantly reduce the total symptom score, or duration of colds. However, for outcomes related to the analgesic effects of NSAID's (headache, ear pain, and muscle and joint pain) NSAID's produced significant benefits. There was no evidence of increased frequency of adverse effects in the NSAID's treatment groups. The authors recommend NSAID's for relieving discomfort or pain caused by the common cold (1357).
3.4.4.10. Zinc
The Cochrane review Zinc and the common cold included 15 randomized controlled double-blind trials. It was concluded, that zinc would shorten the duration of the episode of common cold and also could be used as a prevention so that the risk of developing an episode of common cold would be decreased. It is too early to give general recommendations for the use of zinc as we do not have sufficient knowledge about the optimal dose, formulation and duration of treatment. Further research should focus on the effect of zinc in patients who are at increased risk of developing complications after common cold (recommendation C) (1352,1356).
3.4.4.11. Vitamin C
The role of vitamin C (ascorbic acid) in the prevention and treatment of the common cold has been a subject of controversy for many years, but is widely sold and used as both a preventive and therapeutic agent. A Cochrane study was performed encompassing thirty trials involving 11,350 study participants in the meta-analysis on the relative risk (RR) of developing a cold whilst taking prophylactic vitamin C. The failure of vitamin C supplementation to reduce the incidence of colds in the normal population indicates that routine megadose prophylaxis is not rationally justified for community use. But evidence suggests that it could be justified in people exposed to brief periods of severe physical exercise or cold environments (1366) (Level of evidence Ia, recommendation C).
3.4.4.12. Mucolytics
Mucolytics are used as adjuncts to antibiotic and/or decongestant treatment in ARS in order to reduce the viscosity of sinus secretion. From a recent survey study in France, 45% patients with acute maxillary sinusitis were prescribed with mucolytics (228). Although some drugs have been shown to have mucolytic effect and were recommended as adjunct treatment for ARS, the benefit of such treatment is not clear due to the lack of standardization in pharmacodynamic and pharmacokinetic properties of these drugs, and also doubleblinded, placebo-controlled (DBPC) randomized studies to prove their efficacy.
There is an early RCT study (report in Italian) suggests that bromhexine is superior to placebo (334). In a recent randomized and DBPC study, the use of erdosteine as a mucolytic agent in children with ARS does not directly affect the success of treatment (335). In future, more standardization of mucolytics and larger scale DBPC randomized studies still need to be done in order to fully assess the efficacy of mucolytics in the treatment of ARS.
3.4.4.13. Herbal compounds
There are only a few DBPC randomized studies performed in order to assess the efficacy of herbal compounds in treatment of ARS, which is not representative of the full spectrum of herbal remedies used in the treatment of ARS. More such studies and meta-analysis are needed in order to understanding the pharmacodynamic and pharmacokinetic properties of the active compound from the herbs and their mechanisms in treatment of ARS.
Complementary/alternative medicines are extensively used in the treatment of both ARS and CRS, but evidence-based recommendations are difficult to propose due to the lack of randomized controlled trials and methodological problems in many clinical studies or trials. To date, there are only a few DBPC randomized studies performed in order to assess the efficacy of herbal compounds in treatment of ARS (Table 3.4.7), which is not representative of the full spectrum of herbal remedies used in the treatment of ARS. Also, the active compounds of the herbal compounds have not been discovered, purified and standardized yet. More such studies and meta-analysis are needed in order to understanding the pharmacodynamic and pharmacokinetic properties of the active compound from the herbs and their mechanisms in treatment of ARS. All this information is necessary to allow us to make an evidencebased recommendation, and thus we are unable to accept or reject herbal medicines in the treatment of ARS at present (recommendation C).
In a Cochrane study, the effect of pelargonium sidoides (P. sidoides) extract in treatment of acute respiratory tract infections has been reviewed (336). There was only one study in patients with ARS and another one with the common cold included in analysis based on the RCT criteria (337, 338). In conclusion, P. sidoides may be effective in alleviating symptoms of ARS and the common cold in adults, but doubt exists (336).
The role of vitamin C (ascorbic acid) in the prevention and treatment of the common cold has been a subject of controversy for many years, but is widely sold and used as both a preventive and therapeutic agent. A Cochrane study was performed encompassing thirty trials involving 11,350 study participants in the meta-analysis on the relative risk (RR) of developing a cold whilst taking prophylactic vitamin C. The failure of vitamin C supplementation to reduce the incidence of colds in the normal population indicates that routine megadose prophylaxis is not rationally justified for community use. But evidence suggests that it could be justified in people exposed to brief periods of severe physical exercise or cold environments (1366) (Level of evidence Ia, recommendation C).
3.4.4.12. Mucolytics
Mucolytics are used as adjuncts to antibiotic and/or decongestant treatment in ARS in order to reduce the viscosity of sinus secretion. From a recent survey study in France, 45% patients with acute maxillary sinusitis were prescribed with mucolytics (228). Although some drugs have been shown to have mucolytic effect and were recommended as adjunct treatment for ARS, the benefit of such treatment is not clear due to the lack of standardization in pharmacodynamic and pharmacokinetic properties of these drugs, and also doubleblinded, placebo-controlled (DBPC) randomized studies to prove their efficacy.
There is an early RCT study (report in Italian) suggests that bromhexine is superior to placebo (334). In a recent randomized and DBPC study, the use of erdosteine as a mucolytic agent in children with ARS does not directly affect the success of treatment (335). In future, more standardization of mucolytics and larger scale DBPC randomized studies still need to be done in order to fully assess the efficacy of mucolytics in the treatment of ARS.
3.4.4.13. Herbal compounds
There are only a few DBPC randomized studies performed in order to assess the efficacy of herbal compounds in treatment of ARS, which is not representative of the full spectrum of herbal remedies used in the treatment of ARS. More such studies and meta-analysis are needed in order to understanding the pharmacodynamic and pharmacokinetic properties of the active compound from the herbs and their mechanisms in treatment of ARS.
Complementary/alternative medicines are extensively used in the treatment of both ARS and CRS, but evidence-based recommendations are difficult to propose due to the lack of randomized controlled trials and methodological problems in many clinical studies or trials. To date, there are only a few DBPC randomized studies performed in order to assess the efficacy of herbal compounds in treatment of ARS (Table 3.4.7), which is not representative of the full spectrum of herbal remedies used in the treatment of ARS. Also, the active compounds of the herbal compounds have not been discovered, purified and standardized yet. More such studies and meta-analysis are needed in order to understanding the pharmacodynamic and pharmacokinetic properties of the active compound from the herbs and their mechanisms in treatment of ARS. All this information is necessary to allow us to make an evidencebased recommendation, and thus we are unable to accept or reject herbal medicines in the treatment of ARS at present (recommendation C).
In a Cochrane study, the effect of pelargonium sidoides (P. sidoides) extract in treatment of acute respiratory tract infections has been reviewed (336). There was only one study in patients with ARS and another one with the common cold included in analysis based on the RCT criteria (337, 338). In conclusion, P. sidoides may be effective in alleviating symptoms of ARS and the common cold in adults, but doubt exists (336).
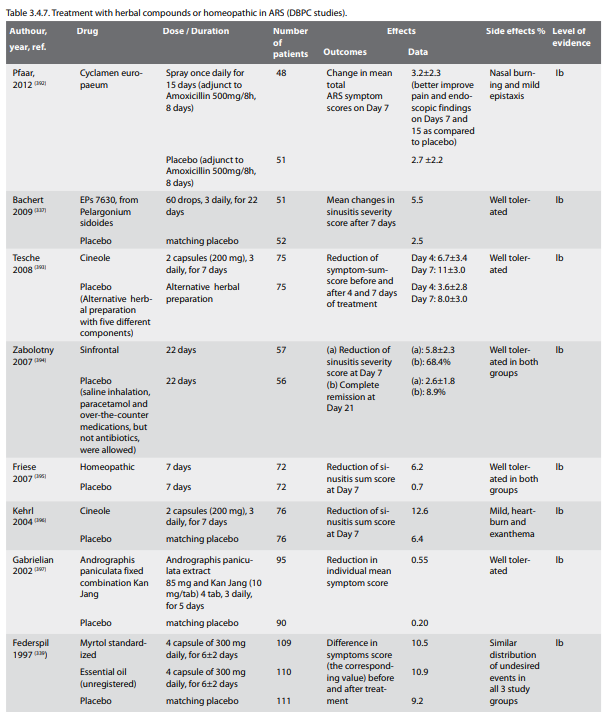
In another DBPC, randomized, multi-centre study (evidence level
Ib), the efficacy of Myrtol standardized (4 capsule of 300
mg/day for 6±2 days) in the treatment of ARS (n=331) was
assessed. The results showed a statistically significant
difference in the improvement of total sinusitis symptoms score,
which had changed by 10.5 and 9.2 points for the treatment with
Myrtol standardized and placebo, respectively (339). A need for
antibiotic treatment after Myrtol was 23%, compared to 40% for
placebo. This drug has been recommended for treatment of ARS and
CRS in the German Society of Oto-Rhino-Laryngology clinical
guidelines (340).
In another Cochrane study the effectiveness and safety of Chinese herbal medicines for the common cold was evaluated. Fourteen studies involving 2440 patients were included. The methods of all studies were rated of poor quality. Included studies used "effective drugs" as controls; however, the efficacy of these control drugs was not reported. In six studies, five herbal preparations were found to be more effective at enhancing recovery than the control; and in the other eight studies, five herbal preparations were shown to be equal to the control. There was a strong probability of different biases in all of the included studies. Chinese herbal medicines may shorten the symptomatic phase in patients with the common cold. However, because of the lack of high quality clinical trials the authors were unable to recommend any kind of Chinese herbal preparation for the common cold (1353).
Also a Cochrane study was performed to determine whether garlic (allium sativum) was effective for either the prevention or treatment of the common cold, when compared to placebo, no treatment or other treatments. There was only one relevant trial that suggested that garlic may prevent occurrences of the common cold, but the authors recommended more studies to validate this finding. Claims of effectiveness appear to rely largely on poor quality evidence (recommendation C)(1356).
3.4.4.14. Cromoglycate
In a randomized double-blind study, comparison was made between sodium cromoglycate and placebo (saline) given as nasal sprays, to control symptoms of post-catarrhal hyperreactive rhinosinusitis (344). There was an improvement in symptoms in about 50% of the patients in each treatment group, but no significant differences between these two treatments in rhinopharyngeal symptoms, ultrasonic scanning of mucosal thickness in the maxillary sinus, or in the patients' evaluation of rhinitis symptoms (evidence level Ib -).
3.4.4.15. Echinacea
There are 10 RCTs performed on the efficacy on Echinacea of wich 5 found that echinacea significantly reduced overall symptom score compared with placebo and 5 RCTs found no significant difference between groups. The weakness of trial methods and differences in interventions make it difficult to draw conclusions about effectiveness (recommendation C)(1365).
3.4.4.8.4. Other Studies without evidence
The is no evidence from RCTs or DBPC studies for other treatments such as anti-mycotics, bacterial lysates, capsaicin, furosemide, proton pump inhibitors, increased fluid intake (1360) and anti-leukotrienes in ARS.
In another Cochrane study the effectiveness and safety of Chinese herbal medicines for the common cold was evaluated. Fourteen studies involving 2440 patients were included. The methods of all studies were rated of poor quality. Included studies used "effective drugs" as controls; however, the efficacy of these control drugs was not reported. In six studies, five herbal preparations were found to be more effective at enhancing recovery than the control; and in the other eight studies, five herbal preparations were shown to be equal to the control. There was a strong probability of different biases in all of the included studies. Chinese herbal medicines may shorten the symptomatic phase in patients with the common cold. However, because of the lack of high quality clinical trials the authors were unable to recommend any kind of Chinese herbal preparation for the common cold (1353).
Also a Cochrane study was performed to determine whether garlic (allium sativum) was effective for either the prevention or treatment of the common cold, when compared to placebo, no treatment or other treatments. There was only one relevant trial that suggested that garlic may prevent occurrences of the common cold, but the authors recommended more studies to validate this finding. Claims of effectiveness appear to rely largely on poor quality evidence (recommendation C)(1356).
3.4.4.14. Cromoglycate
In a randomized double-blind study, comparison was made between sodium cromoglycate and placebo (saline) given as nasal sprays, to control symptoms of post-catarrhal hyperreactive rhinosinusitis (344). There was an improvement in symptoms in about 50% of the patients in each treatment group, but no significant differences between these two treatments in rhinopharyngeal symptoms, ultrasonic scanning of mucosal thickness in the maxillary sinus, or in the patients' evaluation of rhinitis symptoms (evidence level Ib -).
3.4.4.15. Echinacea
There are 10 RCTs performed on the efficacy on Echinacea of wich 5 found that echinacea significantly reduced overall symptom score compared with placebo and 5 RCTs found no significant difference between groups. The weakness of trial methods and differences in interventions make it difficult to draw conclusions about effectiveness (recommendation C)(1365).
3.4.4.8.4. Other Studies without evidence
The is no evidence from RCTs or DBPC studies for other treatments such as anti-mycotics, bacterial lysates, capsaicin, furosemide, proton pump inhibitors, increased fluid intake (1360) and anti-leukotrienes in ARS.
3.5. Complications of ARS
Summary
Orbital, intracranial, and osseous complications of ARS represent rare but potentially serious clinical events. Periorbital complications include preseptal cellulitis, orbital cellulitis, subperiosteal, and intraorbital abscess and their prompt recognition and management (including i.v. antibiotics and drainage, as required) is vital in order to avoid long-term sequelae. Intracranial complications include epidural or subdural abscesses, brain abscess, meningitis, encephalitis, and superior sagittal and cavernous sinus thrombosis. They may present with non specific signs and symptoms and their diagnosis requires a high index of suspicion. Osseous complications result from osteomyelitis of the facial skeleton associated with the progress of inflammation and may present as Potts Puffy tumour or a frontocutaneous fistula.
3.5.1. Introduction
In the pre-antibiotic era, complications of rhinosinusitis represented common and dangerous clinical events. Today, thanks to more reliable diagnostic methods (CT, MRI), improved surgical techniques and the wide range of available antibiotics, their incidence and related mortality have dramatically decreased. In some cases however, if sinus infection is untreated or inadequately treated, complications can still develop (232). Complications of rhinosinusitis are classically defined as orbital, osseous, and endocranial 2 though rarely some unusual complications can develop (Table 3.5.1) (398-402).
3.5.2. Epidemiology of complications
The incidence of ARS complications is approximately 3 per million of population per year and is not reduced by antibiotic prescription
Epidemiological data concerning the complications of rhinosinusitis vary widely and there is no consensus on the exact prevalence of the different types of complications. Moreover, the relationship between ARS or CRS and the various complications is not clearly defined in the literature. In patients hospitalised with sinusitis, the reported rate of complications varies from 3.7%8 to 20% 9, although, by selecting for severe sinus disease, these series clearly overestimate the incidence of complications. Complications are typically classified as orbital (60-75%), intracranial (15-20%) and osseous (5-10%) (403). Overall, sinus disease is the presumed underlying cause of about 10% of intracranial suppuration (404, 405), while sinus disease is related to 10% (preseptal cellulitis) to 90% (orbital cellulitis/ supberiosteal abscess/intraorbital abscess) periorbital infections (406). What is perhaps more clinically relevant is the incidence of complications in patients with acute rhinosinusitis and in the population as whole (Table 3.5.1).
Summary
Orbital, intracranial, and osseous complications of ARS represent rare but potentially serious clinical events. Periorbital complications include preseptal cellulitis, orbital cellulitis, subperiosteal, and intraorbital abscess and their prompt recognition and management (including i.v. antibiotics and drainage, as required) is vital in order to avoid long-term sequelae. Intracranial complications include epidural or subdural abscesses, brain abscess, meningitis, encephalitis, and superior sagittal and cavernous sinus thrombosis. They may present with non specific signs and symptoms and their diagnosis requires a high index of suspicion. Osseous complications result from osteomyelitis of the facial skeleton associated with the progress of inflammation and may present as Potts Puffy tumour or a frontocutaneous fistula.
3.5.1. Introduction
In the pre-antibiotic era, complications of rhinosinusitis represented common and dangerous clinical events. Today, thanks to more reliable diagnostic methods (CT, MRI), improved surgical techniques and the wide range of available antibiotics, their incidence and related mortality have dramatically decreased. In some cases however, if sinus infection is untreated or inadequately treated, complications can still develop (232). Complications of rhinosinusitis are classically defined as orbital, osseous, and endocranial 2 though rarely some unusual complications can develop (Table 3.5.1) (398-402).
3.5.2. Epidemiology of complications
The incidence of ARS complications is approximately 3 per million of population per year and is not reduced by antibiotic prescription
Epidemiological data concerning the complications of rhinosinusitis vary widely and there is no consensus on the exact prevalence of the different types of complications. Moreover, the relationship between ARS or CRS and the various complications is not clearly defined in the literature. In patients hospitalised with sinusitis, the reported rate of complications varies from 3.7%8 to 20% 9, although, by selecting for severe sinus disease, these series clearly overestimate the incidence of complications. Complications are typically classified as orbital (60-75%), intracranial (15-20%) and osseous (5-10%) (403). Overall, sinus disease is the presumed underlying cause of about 10% of intracranial suppuration (404, 405), while sinus disease is related to 10% (preseptal cellulitis) to 90% (orbital cellulitis/ supberiosteal abscess/intraorbital abscess) periorbital infections (406). What is perhaps more clinically relevant is the incidence of complications in patients with acute rhinosinusitis and in the population as whole (Table 3.5.1).
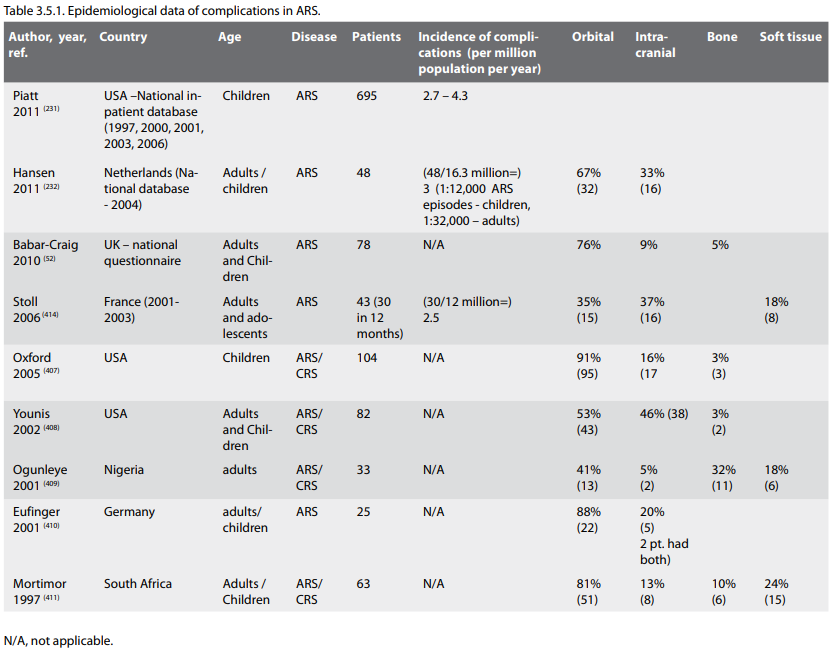
Four studies (attempted to) collect nationwide or large-scale
data: Hansen et al (232), reported 48 ARS complications in 2004
in the Netherlands, corresponding to an incidence of 3 per
million of population per year (or approximately 1 per 12,000
ARS episodes in children and 1 per 36,000 episodes of ARS in
adults). Very similar results were reached by a US study (231)
which recorded an annual incidence of intracranial complications
in children between 2.7 and 4.3 per million per year. A French
study with a 12 million catchment area recorded a yearly
incidence of 2.5 ARS complications per million of population,
excluding paediatric patients (414). In almost all studies males
are significantly more frequently affected than females (231,
232, 412) and ARS was more often the precipitating factor in
children, while CRS with or without NP was more important in
adults (411, 443). In all studies, the commonest complications
were orbital appearing at least twice as often as intracranial
with osseous being the least common (232, 410, 411). There was a
clear seasonal pattern of complications, mirroring the incidence
of URTIs and appearing more often during winter months (231).
While orbital complications tend to occur primarily in small
children, intracranial complications can occur in any age, with
predilection for the second and third decade of life (232, 413).
It is important to note that both the Dutch study (232) and the
study by Babar-Craig (52), which was based on returned
questionnaires by members of the British Rhinology Society and
probably underestimated the incidence of complications, showed
that prescribing of antibiotics for ARS does not prevent the
occurrence of complications. These facts, together with the risk
of antibiotic resistance and of masking intracranial
complications argue strongly against the routine use of
antibiotics in ARS.
The commonest complications of ARS are orbital, appearing approximately twice as often than intracranial and followed by osseous involvement.
The commonest complications of ARS are orbital, appearing approximately twice as often than intracranial and followed by osseous involvement.
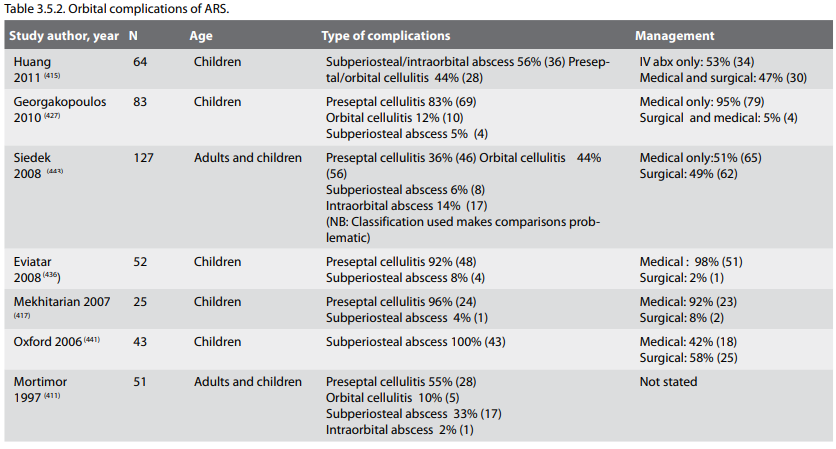
3.5.3. Orbital complications of ARS (Table 3.5.2)
3.5.3.1. Classification
The most common complications of rhinosinusitis are orbital, and they are associated in order of decreasing frequency with the ethmoid, maxillary, frontal and rarely the sphenoid sinus (232, 410, 414-417). The spread of infection directly via the thin and often dehiscent lamina papyracea (416) or by veins (418) occurs with relative ease. It is important to note that orbital complications in children may occur without pain (419).
According to Chandler's classification orbital complications may progress in the following steps (403):
Additionally, cavernous sinus thrombosis as suggested by Mortimer already in 1997 (411) is an intracranial complication and not necessarily the end stage of orbital infection, while it is more often associated with sphenoid (424) rather than ethmoid or frontal sinus infection, which are the most common sources of infection in orbital cellulitis. Periorbital or orbital cellulitis may result from direct or vascular spread of the sinus infection. As the spread of sinus infection through the orbit follows a well-described pattern, the initial manifestations are oedema and erythema of the medial aspects of the eyelid. Spread of infection from the maxillary or frontal sinus produces swelling of the lower or upper eyelid, respectively (425).
The advice of an ophthalmologist should always be sought and objective assessment of proptosis (exophthalmometer), orbital pressure (tonometer), visual acuity, colour vision and eye movements should always be clearly documented (411).
3.5.3.2. Preseptal cellulitis
Preseptal cellulitis (inflammation of the eyelid and conjunctiva) (426) involves the tissue anterior to the orbital septum and is readily seen on CT scan as soft tissue swelling. It occurs often as a complication of upper respiratory tract infection, dacryocystitis or skin infection and less often sinusitis (427-430) and it presents with orbital pain, eyelid oedema, erythema and (sometimes) fever. Typically there is no associated proptosis and no limitation of eye movement, although this may be difficult to assess especially in small children (432). Preseptal cellulitis usually responds to an oral antibiotic but if not aggressively treated, may spread beyond the orbital septum (431). In most cases, preseptal cellulitis is a clinical diagnosis and does not mandate a CT scan (422).
3.5.3.3. Orbital cellulitis
Unlike preseptal cellulitis, orbital cellulitis, orbital abscess and subperiosteal abscess all occur more often as complications of acute rhinosinusitis (427, 429, 432). As the inflammatory changes involve the orbit, proptosis develops together with some limitation of ocular motion, indicating orbital cellulitis. Typical signs are conjunctival oedema (chemosis), a protruding eyeball (proptosis), ocular pain and tenderness, as well as restricted and painful movement of the extraocular muscles (411, 433, 434).
This complication requires aggressive treatment with intravenous antibiotics, as well as the exclusion of subperiosteal or intraorbital abscess.
Any child with proptosis, reduced or painful eye movement (ophthalmoplegia), or decreased visual acuity (initially manifesting itself with reduced green/red colour discrimination) should have a CT scan with i.v. contrast of the sinuses with orbital detail to distinguish between orbital cellulitis and intraorbital or subperiosteal abscess. If a concomitant intracranial complication is suspected or in cases of uncertainty, MRI can provide valuable additional information (435-437). All three conditions (orbital cellulitis, subperiosteal and intraorbital abscess) cause proptosis and limited ocular movement. Evidence of an abscess on the CT scan, progressive orbital findings or vision (especially colour vision) impairment after initial i.v. antibiotic therapy are indications for orbital exploration and drainage. Repeated ophthalmologic examinations of visual acuity should take place and i.v. antibiotic therapy may be converted into oral when the patient has been afebrile for 48 hours and the ophthalmological symptoms and signs are resolving (438).
3.5.3.4. Subperiosteal and orbital abscess
A Subperiosteal abscess forms between the periorbita and the sinuses and is extraconal – i.e. is located outside the ocular muscles. The clinical features of a subperiosteal abscess are oedema, erythema, chemosis and proptosis of the eyelid with limitation of ocular motility and as a consequence of extra-ocular muscle paralysis, the globe becomes fixed (ophthalmoplegia) and visual acuity diminishes. In most series, high fever and raised leucocyte count as well as left turn were strongly associated with (subperiosteal or intraorbital) abscess formation (439).
An orbital abscess is intraconal (contained within the space defined by the ocular muscles) and generally results from diagnostic delay or immunosuppression of the patient (440) with a frequency of between 13% (416) and 8.3% (437) in paediatric studies of orbital complications.
In case of orbital complications, clinical or radiological evidence of an abscess or lack of clinical improvement after 24-48 hours of i.v. antibiotics are indications for prompt surgical exploration and drainage, preferably endoscopic
Investigations. A CT scan of the sinuses with orbital sequences may help to distinguish between cellulitis and orbital or subperiosteal abscess. In the case of a subperiosteal abscess the CT usually reveals oedema of the medial rectus muscle, lateralization of the periorbita, and displacement of the globe downward and laterally. When the CT scan shows obliteration of the detail of the extraocular muscle and the optic nerve by a confluent mass, the orbital cellulitis has progressed to an intraorbital abscess, in which there is sometimes air due to anaerobic bacteria. The predictive accuracy of a clinical diagnosis has been found to be 82% and the accuracy of CT 91%. MRI may be useful in cases of diagnostic uncertainty or when intracranial complications are suspected (408, 441, 442).
Management. Evidence of an abscess on the CT scan or absence of clinical improvement after 24-48 hours of i.v. antibiotics are indications for orbital exploration and drainage (437). An ophthalmologist should check visual acuity from the early stages of the illness. Intravenous antibiotic therapy should cover aerobic and anaerobic pathogens. It can be converted to an oral preparation when the patient has been afebrile for 48 hours (435). Current consensus states that preseptal and orbital cellulitis should be treated with antibiotics while subperiosteal and intraorbital abscesses require surgical exploration (which should include not just the drainage of the abscess but also of the paranasal sinuses (439). In such cases, the consensus is to attempt to drain the abscess endoscopically by opening the lamina papyracea and draining the abscess after completing an endoscopic ethmoidectomy. External approaches to lateral and medial orbital abscesses are also used if necessary (Table 3.5.3).
3.5.3.1. Classification
The most common complications of rhinosinusitis are orbital, and they are associated in order of decreasing frequency with the ethmoid, maxillary, frontal and rarely the sphenoid sinus (232, 410, 414-417). The spread of infection directly via the thin and often dehiscent lamina papyracea (416) or by veins (418) occurs with relative ease. It is important to note that orbital complications in children may occur without pain (419).
According to Chandler's classification orbital complications may progress in the following steps (403):
- (preseptal cellulitis),
-
orbital cellulitis,
-
subperiosteal abscess,
-
orbital abscess, and
-
(cavernous sinus thrombosis)
Additionally, cavernous sinus thrombosis as suggested by Mortimer already in 1997 (411) is an intracranial complication and not necessarily the end stage of orbital infection, while it is more often associated with sphenoid (424) rather than ethmoid or frontal sinus infection, which are the most common sources of infection in orbital cellulitis. Periorbital or orbital cellulitis may result from direct or vascular spread of the sinus infection. As the spread of sinus infection through the orbit follows a well-described pattern, the initial manifestations are oedema and erythema of the medial aspects of the eyelid. Spread of infection from the maxillary or frontal sinus produces swelling of the lower or upper eyelid, respectively (425).
The advice of an ophthalmologist should always be sought and objective assessment of proptosis (exophthalmometer), orbital pressure (tonometer), visual acuity, colour vision and eye movements should always be clearly documented (411).
3.5.3.2. Preseptal cellulitis
Preseptal cellulitis (inflammation of the eyelid and conjunctiva) (426) involves the tissue anterior to the orbital septum and is readily seen on CT scan as soft tissue swelling. It occurs often as a complication of upper respiratory tract infection, dacryocystitis or skin infection and less often sinusitis (427-430) and it presents with orbital pain, eyelid oedema, erythema and (sometimes) fever. Typically there is no associated proptosis and no limitation of eye movement, although this may be difficult to assess especially in small children (432). Preseptal cellulitis usually responds to an oral antibiotic but if not aggressively treated, may spread beyond the orbital septum (431). In most cases, preseptal cellulitis is a clinical diagnosis and does not mandate a CT scan (422).
3.5.3.3. Orbital cellulitis
Unlike preseptal cellulitis, orbital cellulitis, orbital abscess and subperiosteal abscess all occur more often as complications of acute rhinosinusitis (427, 429, 432). As the inflammatory changes involve the orbit, proptosis develops together with some limitation of ocular motion, indicating orbital cellulitis. Typical signs are conjunctival oedema (chemosis), a protruding eyeball (proptosis), ocular pain and tenderness, as well as restricted and painful movement of the extraocular muscles (411, 433, 434).
This complication requires aggressive treatment with intravenous antibiotics, as well as the exclusion of subperiosteal or intraorbital abscess.
Any child with proptosis, reduced or painful eye movement (ophthalmoplegia), or decreased visual acuity (initially manifesting itself with reduced green/red colour discrimination) should have a CT scan with i.v. contrast of the sinuses with orbital detail to distinguish between orbital cellulitis and intraorbital or subperiosteal abscess. If a concomitant intracranial complication is suspected or in cases of uncertainty, MRI can provide valuable additional information (435-437). All three conditions (orbital cellulitis, subperiosteal and intraorbital abscess) cause proptosis and limited ocular movement. Evidence of an abscess on the CT scan, progressive orbital findings or vision (especially colour vision) impairment after initial i.v. antibiotic therapy are indications for orbital exploration and drainage. Repeated ophthalmologic examinations of visual acuity should take place and i.v. antibiotic therapy may be converted into oral when the patient has been afebrile for 48 hours and the ophthalmological symptoms and signs are resolving (438).
3.5.3.4. Subperiosteal and orbital abscess
A Subperiosteal abscess forms between the periorbita and the sinuses and is extraconal – i.e. is located outside the ocular muscles. The clinical features of a subperiosteal abscess are oedema, erythema, chemosis and proptosis of the eyelid with limitation of ocular motility and as a consequence of extra-ocular muscle paralysis, the globe becomes fixed (ophthalmoplegia) and visual acuity diminishes. In most series, high fever and raised leucocyte count as well as left turn were strongly associated with (subperiosteal or intraorbital) abscess formation (439).
An orbital abscess is intraconal (contained within the space defined by the ocular muscles) and generally results from diagnostic delay or immunosuppression of the patient (440) with a frequency of between 13% (416) and 8.3% (437) in paediatric studies of orbital complications.
In case of orbital complications, clinical or radiological evidence of an abscess or lack of clinical improvement after 24-48 hours of i.v. antibiotics are indications for prompt surgical exploration and drainage, preferably endoscopic
Investigations. A CT scan of the sinuses with orbital sequences may help to distinguish between cellulitis and orbital or subperiosteal abscess. In the case of a subperiosteal abscess the CT usually reveals oedema of the medial rectus muscle, lateralization of the periorbita, and displacement of the globe downward and laterally. When the CT scan shows obliteration of the detail of the extraocular muscle and the optic nerve by a confluent mass, the orbital cellulitis has progressed to an intraorbital abscess, in which there is sometimes air due to anaerobic bacteria. The predictive accuracy of a clinical diagnosis has been found to be 82% and the accuracy of CT 91%. MRI may be useful in cases of diagnostic uncertainty or when intracranial complications are suspected (408, 441, 442).
Management. Evidence of an abscess on the CT scan or absence of clinical improvement after 24-48 hours of i.v. antibiotics are indications for orbital exploration and drainage (437). An ophthalmologist should check visual acuity from the early stages of the illness. Intravenous antibiotic therapy should cover aerobic and anaerobic pathogens. It can be converted to an oral preparation when the patient has been afebrile for 48 hours (435). Current consensus states that preseptal and orbital cellulitis should be treated with antibiotics while subperiosteal and intraorbital abscesses require surgical exploration (which should include not just the drainage of the abscess but also of the paranasal sinuses (439). In such cases, the consensus is to attempt to drain the abscess endoscopically by opening the lamina papyracea and draining the abscess after completing an endoscopic ethmoidectomy. External approaches to lateral and medial orbital abscesses are also used if necessary (Table 3.5.3).
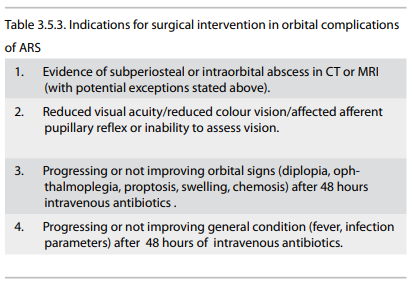
However, there have been a number of recent studies showing good
outcomes with i.v. antibiotics in small children with
subperiosteal abscesses (432, 440, 443). In such cases, and
provided there is:
Prognosis – Follow up. Blindness may result from central retinal artery occlusion, optic neuritis, corneal ulceration, or panophthalmitis. Sepsis not infrequently can spread intracranially as well as anteriorly into the orbit (234).
- clear clinical improvement within 24-48 hours,
- no decrease in visual acuity,
- small (<0.5-1 ml in volume) medially located subperiosteal abscess,
- no significant systemic involvement,
- patient's age is less than 2-4 years,
Prognosis – Follow up. Blindness may result from central retinal artery occlusion, optic neuritis, corneal ulceration, or panophthalmitis. Sepsis not infrequently can spread intracranially as well as anteriorly into the orbit (234).
3.5.4. Endocranial complications
Intracranial complications may present with non-specific symptoms and signs (high fever, headache, lethargy, reduced consciousness) or with focal neurologic or increased intracranial pressure signs
These include epidural or subdural abscesses, brain abscess, meningitis, cerebritis, and superior sagittal and cavernous sinus thrombosis (231, 404, 412, 417, 435, 444).
The clinical presentation of these complications can be nonspecific, being characterized simply by high fever with severe, intractable headache, or even be silent (411, 442). The majority however, usually presents with more specific signs and symptoms that suggest intracranial involvement, such as nausea and vomiting, neck stiffness and altered mental state (234, 411, 412, 440, 445). Intracranial abscesses are often heralded by signs of increased intracranial pressure, meningeal irritation, and focal neurologic deficits, including third, sixth or seventh cranial nerve palsies (411, 423, 440). Although an intracranial abscess can be relatively asymptomatic, subtle affective and behavioural changes often occur showing altered neurologic function, altered consciousness, gait instability, and severe, progressive headache (431, 446).
Endocranial complications are most often associated with frontoethmoidal or sphenoid rhinosinusitis (412). Infections can proceed from the paranasal cavities to the endocranial structures by two different routes: pathogens, starting can pass through the diploic veins to reach the brain; alternatively, they can reach the intracranial structures by eroding the sinus bones or haematologically (445).
All cerebral complications start as encephalitis, but as necrosis and liquefaction of brain tissue progresses, a capsule develops resulting in brain abscess. Studies show a high incidence of anaerobic organisms or mixed aerobic-anaerobic in patients with CNS complications (Table 3.5.4).
A CT scan with contrast is essential for diagnosis as it allows an accurate definition of bone involvement. MRI is increasing being utilised, being more sensitive than CT (448), as well as have an additional value in cavernous sinus thrombosis (412, 445) where an MRI may be necessary (450) or in cases with soft tissue involvement. Moreover, if meningitis is suspected, a lumbar puncture could be useful (445) but only after the exclusion of an abscess using imaging.
High dose long-term i.v. antibiotic therapy followed by burr hole drainage, craniotomy or image guided aspiration as needed, are usually required for successful treatment (451, 452). Combined drainage of the paranasal sinuses (often the frontal sinus) can be performed endoscopically (448), albeit is in no way as a substitute for the drainage of the intracranial abscess (447). Pathogens most commonly involved in the pathogenesis of endocranial complications are Streptococcus and Staphylococcus species and anaerobes (404, 451).
Intracranial complications may present with non-specific symptoms and signs (high fever, headache, lethargy, reduced consciousness) or with focal neurologic or increased intracranial pressure signs
These include epidural or subdural abscesses, brain abscess, meningitis, cerebritis, and superior sagittal and cavernous sinus thrombosis (231, 404, 412, 417, 435, 444).
The clinical presentation of these complications can be nonspecific, being characterized simply by high fever with severe, intractable headache, or even be silent (411, 442). The majority however, usually presents with more specific signs and symptoms that suggest intracranial involvement, such as nausea and vomiting, neck stiffness and altered mental state (234, 411, 412, 440, 445). Intracranial abscesses are often heralded by signs of increased intracranial pressure, meningeal irritation, and focal neurologic deficits, including third, sixth or seventh cranial nerve palsies (411, 423, 440). Although an intracranial abscess can be relatively asymptomatic, subtle affective and behavioural changes often occur showing altered neurologic function, altered consciousness, gait instability, and severe, progressive headache (431, 446).
Endocranial complications are most often associated with frontoethmoidal or sphenoid rhinosinusitis (412). Infections can proceed from the paranasal cavities to the endocranial structures by two different routes: pathogens, starting can pass through the diploic veins to reach the brain; alternatively, they can reach the intracranial structures by eroding the sinus bones or haematologically (445).
All cerebral complications start as encephalitis, but as necrosis and liquefaction of brain tissue progresses, a capsule develops resulting in brain abscess. Studies show a high incidence of anaerobic organisms or mixed aerobic-anaerobic in patients with CNS complications (Table 3.5.4).
A CT scan with contrast is essential for diagnosis as it allows an accurate definition of bone involvement. MRI is increasing being utilised, being more sensitive than CT (448), as well as have an additional value in cavernous sinus thrombosis (412, 445) where an MRI may be necessary (450) or in cases with soft tissue involvement. Moreover, if meningitis is suspected, a lumbar puncture could be useful (445) but only after the exclusion of an abscess using imaging.
High dose long-term i.v. antibiotic therapy followed by burr hole drainage, craniotomy or image guided aspiration as needed, are usually required for successful treatment (451, 452). Combined drainage of the paranasal sinuses (often the frontal sinus) can be performed endoscopically (448), albeit is in no way as a substitute for the drainage of the intracranial abscess (447). Pathogens most commonly involved in the pathogenesis of endocranial complications are Streptococcus and Staphylococcus species and anaerobes (404, 451).
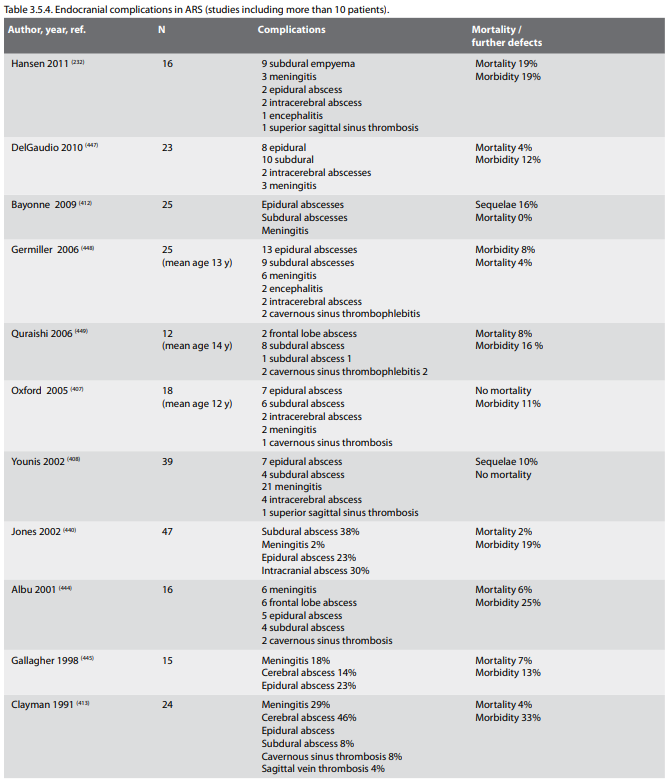
3.5.5. Cavernous sinus thrombosis
When the veins surrounding the paranasal sinuses are affected, further spread can lead to cavernous sinus thrombophlebitis causing sepsis and multiple cranial nerve involvement (431). Such a complication has been estimated at 9% of intracranial complications (444, 445) and is a fortunately rare and dramatic complication of ethmoidal or sphenoidal sinusitis (453).
The main symptoms are bilateral lid drop, exophthalmos, ophthalmic nerve neuralgia, retro-ocular headache with deep pain behind the orbit, complete ophthalmoplegia, papilloedema and signs of meningeal irritation associated with spiking fevers and prostration (425). Full blood count may show increased white blood cell count with neutrophilia and polymorphotcytosis, while lumbar puncture may show non specific meningeal inflammation and blood cultures will help to culture the offending organism (445).
The cornerstone of diagnosis is MR venogram, demonstrating absence of venous flow in the affected cavernous sinus. High-resolution CT scan with contrast can also show filling defects. A mortality rate of 30% and a morbidity rate of 60% remain in the adult population. No data are available for the paediatric population in which the mortality rate for intracranial complications is 10% to 20% (454). The use of anticoagulants in these patients remains controversial (425) but is probably indicated provided imaging shows no evidence of any intracerebral haemorrhagic changes (455). Steroids may help to reduce inflammation and are likely to be helpful, administered with concomitant antibiotics. Drainage of the offending sinus (almost always the sphenoid) is indicated.
When the veins surrounding the paranasal sinuses are affected, further spread can lead to cavernous sinus thrombophlebitis causing sepsis and multiple cranial nerve involvement (431). Such a complication has been estimated at 9% of intracranial complications (444, 445) and is a fortunately rare and dramatic complication of ethmoidal or sphenoidal sinusitis (453).
The main symptoms are bilateral lid drop, exophthalmos, ophthalmic nerve neuralgia, retro-ocular headache with deep pain behind the orbit, complete ophthalmoplegia, papilloedema and signs of meningeal irritation associated with spiking fevers and prostration (425). Full blood count may show increased white blood cell count with neutrophilia and polymorphotcytosis, while lumbar puncture may show non specific meningeal inflammation and blood cultures will help to culture the offending organism (445).
The cornerstone of diagnosis is MR venogram, demonstrating absence of venous flow in the affected cavernous sinus. High-resolution CT scan with contrast can also show filling defects. A mortality rate of 30% and a morbidity rate of 60% remain in the adult population. No data are available for the paediatric population in which the mortality rate for intracranial complications is 10% to 20% (454). The use of anticoagulants in these patients remains controversial (425) but is probably indicated provided imaging shows no evidence of any intracerebral haemorrhagic changes (455). Steroids may help to reduce inflammation and are likely to be helpful, administered with concomitant antibiotics. Drainage of the offending sinus (almost always the sphenoid) is indicated.
3.5.6. Bone complications
Sinus infection can also extend to the bone producing osteomyelitis and eventually involving the brain and nervous system. Even if the most frequent intracranial spread is due to frontal sinusitis, any sinus infection can lead to such a complication (425). The most common osseous complications are osteomyelitis of the maxillary (typically in infancy) or frontal bones (398).
As vascular necrosis results from frontal sinus osteitis, an osteomyelitis of the anterior or posterior table of the frontal sinus is evident. On the anterior wall it presents clinically with "doughy" oedema of the skin over the frontal bone producing a mass (Pott's puffy tumour) whereas from the posterior wall spread occurs directly or via thrombophlebitis of the valveless diploic veins leading to meningitis, peridural abscess or brain abscess (425). The infection can proceed anteriorly by breaching.
In this context, Gallagher (445) reviewed the files of 125 patients with complicated rhinosinusitis and found that osteomyelitis developed in about 9% of cases. The sinus walls were affected in 32% of patients in Ogunleye's data (409). Lang in 2001 recorded 10 cases of subdural empyema in adults and children secondary to frontal sinus infection: among them four had Pott's puffy tumour and one had periorbital abscess (456).
Signs and symptoms of intracranial involvement are soft tissue oedema (especially of the superior lid), high fever, severe headache, meningeal irritation, nausea and vomiting, diplopia, photophobia, papillary oedema, coma and focal neurological signs. Ocular signs can appear contra laterally. Contrastenhanced CT scan confirms the diagnosis. A lumbar puncture, though contraindicated if intracranial pressure is elevated, can also be useful.
Therapy includes a combination of i.v. broad-spectrum antibiotics administration and surgical debridement of sequestered bone and drainage (425).
Management of ARS complications is always multidisciplinary – the advice of an ophthalmologist in cases of orbital involvement and of neurologist/neurosurgeon in intracranial involvement is mandatory
Sinus infection can also extend to the bone producing osteomyelitis and eventually involving the brain and nervous system. Even if the most frequent intracranial spread is due to frontal sinusitis, any sinus infection can lead to such a complication (425). The most common osseous complications are osteomyelitis of the maxillary (typically in infancy) or frontal bones (398).
As vascular necrosis results from frontal sinus osteitis, an osteomyelitis of the anterior or posterior table of the frontal sinus is evident. On the anterior wall it presents clinically with "doughy" oedema of the skin over the frontal bone producing a mass (Pott's puffy tumour) whereas from the posterior wall spread occurs directly or via thrombophlebitis of the valveless diploic veins leading to meningitis, peridural abscess or brain abscess (425). The infection can proceed anteriorly by breaching.
In this context, Gallagher (445) reviewed the files of 125 patients with complicated rhinosinusitis and found that osteomyelitis developed in about 9% of cases. The sinus walls were affected in 32% of patients in Ogunleye's data (409). Lang in 2001 recorded 10 cases of subdural empyema in adults and children secondary to frontal sinus infection: among them four had Pott's puffy tumour and one had periorbital abscess (456).
Signs and symptoms of intracranial involvement are soft tissue oedema (especially of the superior lid), high fever, severe headache, meningeal irritation, nausea and vomiting, diplopia, photophobia, papillary oedema, coma and focal neurological signs. Ocular signs can appear contra laterally. Contrastenhanced CT scan confirms the diagnosis. A lumbar puncture, though contraindicated if intracranial pressure is elevated, can also be useful.
Therapy includes a combination of i.v. broad-spectrum antibiotics administration and surgical debridement of sequestered bone and drainage (425).
Management of ARS complications is always multidisciplinary – the advice of an ophthalmologist in cases of orbital involvement and of neurologist/neurosurgeon in intracranial involvement is mandatory
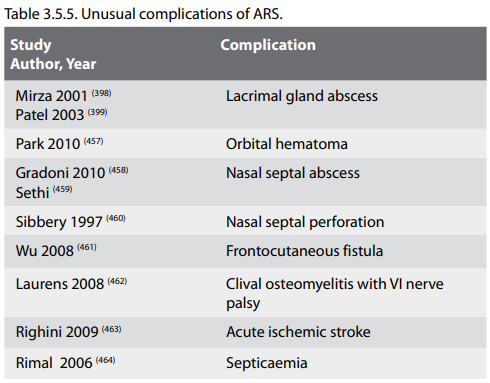
3.5.7. Unusual complications of rhinosinusitis
3.5.8. Follow-up of complications
It is important to note that some complications may occasionally appear simultaneously (for example Potts Puffy tumour and intracranial extension, orbital and intracranial complications). A follow up of such patients for a minimum of 6 months is advised, in order to monitor for complete resolution of disease as well as exclude disease recurrence or any complication of treatment.
3.6. Paediatric ARS
Summary
ARS in children is a common entity that usually occurs in the context of an upper respiratory viral illness. In the children where this illness is not self-limited and extends beyond 7-10 days, many agree that a bacterial infection is likely. The diagnosis is mostly based on history of symptoms and their duration as well as physical findings. In most cases this is a self-limited process but, treatment with antibiotics seems to accelerate resolution. Whether this benefit outweighs the risks associated with frequent antibiotic prescriptions remains to be clarified. Intranasal steroids might be useful adjuncts to antibiotics in the treatment of ARS and very limited evidence in older children suggests that they may be useful as a single agent in the treatment. Ancillary therapy in the form of nasal irrigations, antihistamines, decongestants, or mucolytics have not been shown to be helpful.
3.6.1. Definition of ARS in children
ARS is most often viral in aetiology and self-limited.
Acute rhinosinusitis in children is defined as the sudden onset of two or more of the symptoms (discoloured nasal discharge, nasal blockage/obstruction/ congestion, cough at daytime and night-time) for less than 12 weeks, with validation by telephone or interview. Symptom free intervals may exist if the problem is recurrent.
As in adults, common cold / viral ARS is defined as duration of symptoms for less than 10 days; post-viral ARS as increase of symptoms after 5 days or persistent symptoms after 10 days; and suggestive of ABRS when are present at least 3 symptoms/signs among discoloured discharge (with unilateral predominance) and purulent secretion in cavum nasi, severe local pain (with unilateral predominance), fever (>38ºC), elevated ESR/CRP, and double sickening (i.e. a deterioration after an initial milder phase of illness) (see also chapter 2).
3.6.2. Paranasal Sinus Development
Not all sinuses are well developed at birth. The frontal sinuses are indistinguishable from the anterior ethmoid cells and they grow slowly after birth so that they are barely seen anatomically at 1 year of age. After the fourth year, the frontal sinuses begin to enlarge and can usually be demonstrated radiographically in around 20-30% of children at age 6 years (465). Their size continues to increase into the late teens and more than 85% of children will show pneumatized frontal sinuses on CT scanning at the age of 12 years (465). When volume estimates are generated from examining 3D reconstructions of CT scans, the volume is around 2 ml around age 10 years and reaches adult size around age 19 with mean volume after full growth being 3.46 ml (466).
At birth, the ethmoid and maxillary sinuses are the only sinuses that are large enough to be clinically significant as a cause of rhinosinusitis. In one study, more than 90% of subjects showed radiographically visible ethmoid sinuses at birth (465). The ethmoid sinuses rapidly increase in size until 7 years of age and complete their growth by age 15-16 years with a mean volume after full growth averaging 4.51 ml (466). The maxillary sinuses are usually pneumatized at birth and the volume in patients at 2 years of age is around 2 ml (466). The sinus grows rapidly reaching around 10 ml in volume around age 9 years and full growth volume by 15 years averaging 14.8 ml. Much of the growth that occurs after the twelfth year is in the inferior direction with pneumatisation of the alveolar process after eruption of the secondary dentition. By adulthood, the floor of the maxillary sinus is usually 4-5 mm inferior to the floor of the nasal cavity.
At birth, the size of the sphenoid sinus is small and is little more than an evagination of the sphenoethmoidal recess. By the age of 7 years, the sphenoid sinuses have extended posteriorly to the level of the sella turcica and over 85% of patients have pneumatized sphenoid sinuses visualized on CT scanning by age 8 years (465). The sphenoid sinuses exhibit a growth spurt between 6-10 years of age and growth is completed by the age of 15 years with the mean volume after full growth averaging 3.47 ml (466). By the late teens, most of the sphenoid sinuses have aerated to the dorsum sellae and some further enlargement may occur in adults.
3.6.3. Classification and diagnosis
The clinical diagnosis of ARS in children is challenging related to the overlap of symptoms with other common childhood nasal diseases such as viral upper respiratory tract infections and allergic rhinitis as well as the challenges related to physical examination. The symptoms are often subtle and the history is limited to the observations and subjective evaluation by the child's parent. Because some younger children might not tolerate nasal endoscopy, clinicians are sometimes hindered in their physical examination and have to rely on history and or imaging studies for appropriate diagnosis.
Symptom profiles of ARS in children include fever (50-60%), rhinorrhoea (71-80%), cough (50-80%), and pain (29-33%) (8). In a recent study of 69 children between the ages of 3 and 12 years, ARS was diagnosed by purulent nasal drainage for more than 7 days and abnormal findings in the maxillary sinuses on Water's projection. In these children, the most troublesome symptoms were postnasal drip, nasal obstruction, and cough (76). In a mail survey of American general pediatricians, symptoms thought to be very important in the diagnosis of ARS included prolonged symptom duration, purulent rhinorrhoea, and nasal congestion (230).
In children, ARS most often presents as either a severe upper respiratory tract illness with fever >39°C, purulent rhinorrhoea and facial pain or, more commonly, as a prolonged URTI with chronic cough and nasal discharge. In a study of the relationship between symptoms of acute respiratory infection and objective changes within the sinuses utilizing MRI scans, 60 children (mean age=5.7 yrs.) were investigated who had symptoms for an average of 6 days before scanning (467). Approximately 60% of the children had abnormalities in their maxillary and ethmoid sinuses, 35% in the sphenoid sinuses, and 18% in the frontal sinuses. In 26 children with major abnormalities, a follow up MRI scan taken 2 weeks later showed a significant reduction in the extent of abnormalities irrespective of resolution of clinical symptoms. This study reinforces the notion that, like in adults, every upper respiratory tract infection is essentially an episode of rhinosinusitis with common involvement of the paranasal sinuses by the viral process.
Few viral ARS episodes progress to bacterial ARS.
Despite the lack of good studies, most clinicians and investigators agree that the diagnosis of bacterial ARS can be made after a viral URTI when children have persistent URI symptoms for >10 days without improvement (nasal discharge, daytime cough worsening at night) or an abrupt increase in severity of symptoms after initial improvement of symptoms of a URTI, or a URTI that seems more severe than usual (high fever, copious purulent nasal discharge, periorbital oedema and pain) (8 , 96, 468).
In a longitudinal study of 112 children aged 6-35 months, 623 URTIs were observed over a 3-year period and episodes of sinusitis as defined above were documented by the investigators (31). Eight percent of the URIs were complicated by sinusitis, with 29% of the episodes diagnosed because of an increase in the severity of symptoms before 10 days of illness and the remaining diagnosed on the basis of persistent symptoms beyond 10 days. The occurrence of sinusitis in the context of URIs was 7% in the 6-11 month age group and in children over 24 months, and 10% in children who were 12-23 months old. In an older, but similar, study, 159 full term infants were followed prospectively for a 3 year period and the frequency of URIs and complicating sinusitis were evaluated (469). The authors calculated the percentage of children experiencing symptoms beyond 2 standard deviations from the mean duration of respiratory symptoms (in days) and took that as an indicator of ARS. This value varied with age and ranged between 16 and 22 days. The incidence based on these assumptions ranged between 4 and 7.3% and was highest for children in their first year of life and in day care. On average, a child younger than 5 years of age has 2 to 7 episodes of URTI per year (470, 471), and a child attending day care may have up to 14 episodes per year (472). With the incidence rates reported above, the number of acute sinusitis episodes in children every year is sizeable.
Distinguishing between ARS and CRS is based on duration of illness in both children and adults. ARS is defined by symptoms lasting <12 weeks with complete resolution of symptoms. Symptoms lasting ≥12 weeks without complete resolution of symptoms are consistent with CRS. A very common clinical scenario in children presenting to the otorhinolaryngologist's office is that of CRS with upper respiratory tract infectioninduced acute exacerbations.
3.5.8. Follow-up of complications
It is important to note that some complications may occasionally appear simultaneously (for example Potts Puffy tumour and intracranial extension, orbital and intracranial complications). A follow up of such patients for a minimum of 6 months is advised, in order to monitor for complete resolution of disease as well as exclude disease recurrence or any complication of treatment.
3.6. Paediatric ARS
Summary
ARS in children is a common entity that usually occurs in the context of an upper respiratory viral illness. In the children where this illness is not self-limited and extends beyond 7-10 days, many agree that a bacterial infection is likely. The diagnosis is mostly based on history of symptoms and their duration as well as physical findings. In most cases this is a self-limited process but, treatment with antibiotics seems to accelerate resolution. Whether this benefit outweighs the risks associated with frequent antibiotic prescriptions remains to be clarified. Intranasal steroids might be useful adjuncts to antibiotics in the treatment of ARS and very limited evidence in older children suggests that they may be useful as a single agent in the treatment. Ancillary therapy in the form of nasal irrigations, antihistamines, decongestants, or mucolytics have not been shown to be helpful.
3.6.1. Definition of ARS in children
ARS is most often viral in aetiology and self-limited.
Acute rhinosinusitis in children is defined as the sudden onset of two or more of the symptoms (discoloured nasal discharge, nasal blockage/obstruction/ congestion, cough at daytime and night-time) for less than 12 weeks, with validation by telephone or interview. Symptom free intervals may exist if the problem is recurrent.
As in adults, common cold / viral ARS is defined as duration of symptoms for less than 10 days; post-viral ARS as increase of symptoms after 5 days or persistent symptoms after 10 days; and suggestive of ABRS when are present at least 3 symptoms/signs among discoloured discharge (with unilateral predominance) and purulent secretion in cavum nasi, severe local pain (with unilateral predominance), fever (>38ºC), elevated ESR/CRP, and double sickening (i.e. a deterioration after an initial milder phase of illness) (see also chapter 2).
3.6.2. Paranasal Sinus Development
Not all sinuses are well developed at birth. The frontal sinuses are indistinguishable from the anterior ethmoid cells and they grow slowly after birth so that they are barely seen anatomically at 1 year of age. After the fourth year, the frontal sinuses begin to enlarge and can usually be demonstrated radiographically in around 20-30% of children at age 6 years (465). Their size continues to increase into the late teens and more than 85% of children will show pneumatized frontal sinuses on CT scanning at the age of 12 years (465). When volume estimates are generated from examining 3D reconstructions of CT scans, the volume is around 2 ml around age 10 years and reaches adult size around age 19 with mean volume after full growth being 3.46 ml (466).
At birth, the ethmoid and maxillary sinuses are the only sinuses that are large enough to be clinically significant as a cause of rhinosinusitis. In one study, more than 90% of subjects showed radiographically visible ethmoid sinuses at birth (465). The ethmoid sinuses rapidly increase in size until 7 years of age and complete their growth by age 15-16 years with a mean volume after full growth averaging 4.51 ml (466). The maxillary sinuses are usually pneumatized at birth and the volume in patients at 2 years of age is around 2 ml (466). The sinus grows rapidly reaching around 10 ml in volume around age 9 years and full growth volume by 15 years averaging 14.8 ml. Much of the growth that occurs after the twelfth year is in the inferior direction with pneumatisation of the alveolar process after eruption of the secondary dentition. By adulthood, the floor of the maxillary sinus is usually 4-5 mm inferior to the floor of the nasal cavity.
At birth, the size of the sphenoid sinus is small and is little more than an evagination of the sphenoethmoidal recess. By the age of 7 years, the sphenoid sinuses have extended posteriorly to the level of the sella turcica and over 85% of patients have pneumatized sphenoid sinuses visualized on CT scanning by age 8 years (465). The sphenoid sinuses exhibit a growth spurt between 6-10 years of age and growth is completed by the age of 15 years with the mean volume after full growth averaging 3.47 ml (466). By the late teens, most of the sphenoid sinuses have aerated to the dorsum sellae and some further enlargement may occur in adults.
3.6.3. Classification and diagnosis
The clinical diagnosis of ARS in children is challenging related to the overlap of symptoms with other common childhood nasal diseases such as viral upper respiratory tract infections and allergic rhinitis as well as the challenges related to physical examination. The symptoms are often subtle and the history is limited to the observations and subjective evaluation by the child's parent. Because some younger children might not tolerate nasal endoscopy, clinicians are sometimes hindered in their physical examination and have to rely on history and or imaging studies for appropriate diagnosis.
Symptom profiles of ARS in children include fever (50-60%), rhinorrhoea (71-80%), cough (50-80%), and pain (29-33%) (8). In a recent study of 69 children between the ages of 3 and 12 years, ARS was diagnosed by purulent nasal drainage for more than 7 days and abnormal findings in the maxillary sinuses on Water's projection. In these children, the most troublesome symptoms were postnasal drip, nasal obstruction, and cough (76). In a mail survey of American general pediatricians, symptoms thought to be very important in the diagnosis of ARS included prolonged symptom duration, purulent rhinorrhoea, and nasal congestion (230).
In children, ARS most often presents as either a severe upper respiratory tract illness with fever >39°C, purulent rhinorrhoea and facial pain or, more commonly, as a prolonged URTI with chronic cough and nasal discharge. In a study of the relationship between symptoms of acute respiratory infection and objective changes within the sinuses utilizing MRI scans, 60 children (mean age=5.7 yrs.) were investigated who had symptoms for an average of 6 days before scanning (467). Approximately 60% of the children had abnormalities in their maxillary and ethmoid sinuses, 35% in the sphenoid sinuses, and 18% in the frontal sinuses. In 26 children with major abnormalities, a follow up MRI scan taken 2 weeks later showed a significant reduction in the extent of abnormalities irrespective of resolution of clinical symptoms. This study reinforces the notion that, like in adults, every upper respiratory tract infection is essentially an episode of rhinosinusitis with common involvement of the paranasal sinuses by the viral process.
Few viral ARS episodes progress to bacterial ARS.
Despite the lack of good studies, most clinicians and investigators agree that the diagnosis of bacterial ARS can be made after a viral URTI when children have persistent URI symptoms for >10 days without improvement (nasal discharge, daytime cough worsening at night) or an abrupt increase in severity of symptoms after initial improvement of symptoms of a URTI, or a URTI that seems more severe than usual (high fever, copious purulent nasal discharge, periorbital oedema and pain) (8 , 96, 468).
In a longitudinal study of 112 children aged 6-35 months, 623 URTIs were observed over a 3-year period and episodes of sinusitis as defined above were documented by the investigators (31). Eight percent of the URIs were complicated by sinusitis, with 29% of the episodes diagnosed because of an increase in the severity of symptoms before 10 days of illness and the remaining diagnosed on the basis of persistent symptoms beyond 10 days. The occurrence of sinusitis in the context of URIs was 7% in the 6-11 month age group and in children over 24 months, and 10% in children who were 12-23 months old. In an older, but similar, study, 159 full term infants were followed prospectively for a 3 year period and the frequency of URIs and complicating sinusitis were evaluated (469). The authors calculated the percentage of children experiencing symptoms beyond 2 standard deviations from the mean duration of respiratory symptoms (in days) and took that as an indicator of ARS. This value varied with age and ranged between 16 and 22 days. The incidence based on these assumptions ranged between 4 and 7.3% and was highest for children in their first year of life and in day care. On average, a child younger than 5 years of age has 2 to 7 episodes of URTI per year (470, 471), and a child attending day care may have up to 14 episodes per year (472). With the incidence rates reported above, the number of acute sinusitis episodes in children every year is sizeable.
Distinguishing between ARS and CRS is based on duration of illness in both children and adults. ARS is defined by symptoms lasting <12 weeks with complete resolution of symptoms. Symptoms lasting ≥12 weeks without complete resolution of symptoms are consistent with CRS. A very common clinical scenario in children presenting to the otorhinolaryngologist's office is that of CRS with upper respiratory tract infectioninduced acute exacerbations.
3.6.4. Differential diagnosis
When a child presents with symptoms of ARS as listed above, the differential diagnosis must include intranasal foreign body and unilateral choanal stenosis. In these entities, the symptoms are usually unilateral and can be relatively easily differentiated clinically from ARS by history and physical examination, including nasal endoscopy. AR will usually not manifest with purulent drainage as part of the clinical presentation. Adenoiditis can have a very similar clinical presentation including anterior and posterior purulent drainage and cough and is very relevant in the differential diagnosis in the paediatric age group. In a study of adenoid size evaluated by MRI in a patient cohort with no symptoms related to the adenoids or adenoid disease, adenoid size was larger in the paediatric age group and declined with advancing age (473). Peak size was between 7 and 10 years of age and largest dimensions were in the 4-15 years age group. In an attempt to differentiate between adenoiditis and ARS based on endoscopic findings, Marseglia and colleagues performed a cross sectional study of 287 consecutive children in whom ARS was suspected based on symptoms lasting for more than 10 days (270). Nasal endoscopy was performed and the diagnosis of ARS was made if purulent discharge was identified in the ostiomeatal or sphenoethmoidal areas, and the diagnosis of adenoiditis was made if there was purulent drainage over the adenoids. Based on those criteria, rhinosinusitis was confirmed in 89.2% of the patients and was isolated in 80.8% and coupled with adenoiditis in 19.2%. Adenoiditis alone was confirmed in 7% of the cohort. Combined involvement of the sinuses and adenoids was more frequent in younger patients (2-5 years age group) whereas isolated rhinosinusitis was more frequent in older children. Although this study can be criticized by the manner in which the diagnosis was made as one would expect drainage from the sinuses to involve the adenoids as it moves posteriorly in the nose, and the lack of a more objective measure to diagnose rhinosinusitis such as a CT scan, the data supports the high coexistence of infection of the adenoids and the paranasal sinuses in the above clinical context. It is also evident that based on clinical presentation alone, the differentiation between adenoiditis and ARS in children is very difficult.
3.6.5. Bacteriology
Wald et al. studied the bacteriology of ARS in 1981 (474). They obtained cultures from children with maxillary sinus opacification documented by Water's X-ray by means of sinus taps and found that S. pneumoniae, H. influenzae, and M. catarrhalis were the organisms most frequently isolated from maxillary sinus aspirates in these children. Several studies since then have confirmed that the most common organisms responsible for bacterial ARS in children are S. pneumoniae, H. influenza, M. catarrhalis, S. pyogenes, and anaerobes (8). Unlike the visit rate for acute otitis media in children younger than 18 years, which has decreased between 1998 and 2007 following the introduction of the heptavalent pneumococcal conjugate vaccine in the United States, the visit rate for ARS has remained stable at 11-14 visits per 1000 children (475). In a later study, Hwang et al performed a retrospective review of all paediatric patients requiring intervention for ARS over a seven-year period (476). They reported that instead of the common bacteria noted above, S. viridans was the major culprit in sinus cultures. Brook et al. found anaerobic bacteria in acute infections as well, however, these organisms are most frequently seen in maxillary CRS due to odontogenic causes. The predominant anaerobic bacteria were gram-negative bacilli such as Peptostreptococcus and Fusobacterium (477, 478).
3.6.6. Diagnostic Workup
A complete physical exam should follow a carefully obtained medical and family history. The nasal exam in children should begin with anterior rhinoscopy examining the middle meatus, inferior turbinates, mucosal character, and presence of purulent drainage. This is often accomplished easily using the largest speculum of an otoscope, or alternatively, a head light and nasal speculum. Topical decongestion may be used to improve visualization. Nasal endoscopy that will allow superior visualization of the middle meatus, adenoid bed, and nasopharynx is strongly recommended in children who are able to tolerate the examination. An oral cavity exam may reveal purulent postnasal drainage, cobblestoning of the posterior pharyngeal wall, or tonsillar hypertrophy
Obtaining a culture is usually not necessary in the context of uncomplicated ARS. Obtaining a culture might be useful in patients who have not responded to conventional medical treatment within 48-72 hours, in immune-compromised patients, in the presence of complications, and if the child presents with severe illness and appears toxic (8, 479). Although the golden standard would be a maxillary sinus tap, this is a relatively invasive procedure, and is difficult to perform in a child in the office. Middle meatal cultures under endoscopic visualization have shown promise in correlating with antral cultures. In children, data regarding the usefulness of this approach are limited and are mostly based on studies in CRS and will be discussed in the relevant chapter.
While the diagnosis of ARS in the paediatric population is generally made on clinical grounds, computed tomography (CT) is the imaging modality of choice (279). The recommendations of the American Academy of Paediatrics, published in 2001, state that CT should be reserved for those patients with symptoms persisting after 10 days of appropriate therapy and in patients with suspected complications (especially in the brain and in the orbit) (96). In children with the clinical diagnosis of rhinosinusitis, the most commonly involved sinus is the maxillary sinus (99%) followed by the ethmoid sinus (91%) (480). MRI of the sinuses, orbits, and brain should be performed whenever complications of rhinosinusitis are suspected.
When a child presents with symptoms of ARS as listed above, the differential diagnosis must include intranasal foreign body and unilateral choanal stenosis. In these entities, the symptoms are usually unilateral and can be relatively easily differentiated clinically from ARS by history and physical examination, including nasal endoscopy. AR will usually not manifest with purulent drainage as part of the clinical presentation. Adenoiditis can have a very similar clinical presentation including anterior and posterior purulent drainage and cough and is very relevant in the differential diagnosis in the paediatric age group. In a study of adenoid size evaluated by MRI in a patient cohort with no symptoms related to the adenoids or adenoid disease, adenoid size was larger in the paediatric age group and declined with advancing age (473). Peak size was between 7 and 10 years of age and largest dimensions were in the 4-15 years age group. In an attempt to differentiate between adenoiditis and ARS based on endoscopic findings, Marseglia and colleagues performed a cross sectional study of 287 consecutive children in whom ARS was suspected based on symptoms lasting for more than 10 days (270). Nasal endoscopy was performed and the diagnosis of ARS was made if purulent discharge was identified in the ostiomeatal or sphenoethmoidal areas, and the diagnosis of adenoiditis was made if there was purulent drainage over the adenoids. Based on those criteria, rhinosinusitis was confirmed in 89.2% of the patients and was isolated in 80.8% and coupled with adenoiditis in 19.2%. Adenoiditis alone was confirmed in 7% of the cohort. Combined involvement of the sinuses and adenoids was more frequent in younger patients (2-5 years age group) whereas isolated rhinosinusitis was more frequent in older children. Although this study can be criticized by the manner in which the diagnosis was made as one would expect drainage from the sinuses to involve the adenoids as it moves posteriorly in the nose, and the lack of a more objective measure to diagnose rhinosinusitis such as a CT scan, the data supports the high coexistence of infection of the adenoids and the paranasal sinuses in the above clinical context. It is also evident that based on clinical presentation alone, the differentiation between adenoiditis and ARS in children is very difficult.
3.6.5. Bacteriology
Wald et al. studied the bacteriology of ARS in 1981 (474). They obtained cultures from children with maxillary sinus opacification documented by Water's X-ray by means of sinus taps and found that S. pneumoniae, H. influenzae, and M. catarrhalis were the organisms most frequently isolated from maxillary sinus aspirates in these children. Several studies since then have confirmed that the most common organisms responsible for bacterial ARS in children are S. pneumoniae, H. influenza, M. catarrhalis, S. pyogenes, and anaerobes (8). Unlike the visit rate for acute otitis media in children younger than 18 years, which has decreased between 1998 and 2007 following the introduction of the heptavalent pneumococcal conjugate vaccine in the United States, the visit rate for ARS has remained stable at 11-14 visits per 1000 children (475). In a later study, Hwang et al performed a retrospective review of all paediatric patients requiring intervention for ARS over a seven-year period (476). They reported that instead of the common bacteria noted above, S. viridans was the major culprit in sinus cultures. Brook et al. found anaerobic bacteria in acute infections as well, however, these organisms are most frequently seen in maxillary CRS due to odontogenic causes. The predominant anaerobic bacteria were gram-negative bacilli such as Peptostreptococcus and Fusobacterium (477, 478).
3.6.6. Diagnostic Workup
A complete physical exam should follow a carefully obtained medical and family history. The nasal exam in children should begin with anterior rhinoscopy examining the middle meatus, inferior turbinates, mucosal character, and presence of purulent drainage. This is often accomplished easily using the largest speculum of an otoscope, or alternatively, a head light and nasal speculum. Topical decongestion may be used to improve visualization. Nasal endoscopy that will allow superior visualization of the middle meatus, adenoid bed, and nasopharynx is strongly recommended in children who are able to tolerate the examination. An oral cavity exam may reveal purulent postnasal drainage, cobblestoning of the posterior pharyngeal wall, or tonsillar hypertrophy
Obtaining a culture is usually not necessary in the context of uncomplicated ARS. Obtaining a culture might be useful in patients who have not responded to conventional medical treatment within 48-72 hours, in immune-compromised patients, in the presence of complications, and if the child presents with severe illness and appears toxic (8, 479). Although the golden standard would be a maxillary sinus tap, this is a relatively invasive procedure, and is difficult to perform in a child in the office. Middle meatal cultures under endoscopic visualization have shown promise in correlating with antral cultures. In children, data regarding the usefulness of this approach are limited and are mostly based on studies in CRS and will be discussed in the relevant chapter.
While the diagnosis of ARS in the paediatric population is generally made on clinical grounds, computed tomography (CT) is the imaging modality of choice (279). The recommendations of the American Academy of Paediatrics, published in 2001, state that CT should be reserved for those patients with symptoms persisting after 10 days of appropriate therapy and in patients with suspected complications (especially in the brain and in the orbit) (96). In children with the clinical diagnosis of rhinosinusitis, the most commonly involved sinus is the maxillary sinus (99%) followed by the ethmoid sinus (91%) (480). MRI of the sinuses, orbits, and brain should be performed whenever complications of rhinosinusitis are suspected.
3.6.7. Medical Treatment of Acute Rhinosinusitis
Most episodes of ARS are self-limited and will resolve spontaneously.
3.6.7.1. Antibiotics
Antibiotics are the most frequently used therapeutic agents in ARS (Table 3.6.1). Published trials in children and adults were reviewed in a recent meta-analysis of randomized controlled trials evaluating antibiotic treatment for ARS in which 3 of the 17 evaluated studies were performed in the paediatric age group (345). In total, 3291 outpatients (2915 adults and 376 children) were treated in the trials included in the meta-analysis. The diagnosis of ARS in the trials was based on clinical criteria in most studies and radiologic and other laboratory criteria in the rest. In most studies, inclusion of patients with viral upper respiratory tract infections was avoided by enrolling patients whose symptoms were of more than 7-10 days duration. The results suggest that, compared with placebo, antibiotics were associated with a higher rate of cure or improvement within 7-15 days with the rate of resolution of symptoms being faster with antibiotics in most randomized controlled trials. The overall positive effect in favour of antibiotics was significant but modest. No difference in cure was found when a subgroup analysis was performed for age. A more recent randomized, placebo-controlled trial not included in the meta-analysis evaluated the efficacy of amoxicillin (90 mg/kg) with potassium clavulanate (6.4 mg/kg) or placebo in children 1-10 years of age with a clinical presentation compatible with bacterial ARS (persistent symptoms, acutely worsening symptoms or severe symptoms) (351). Symptom scores were obtained at multiple time points and the children were evaluated at day 14 from onset of treatment and their condition rated as cured, improved, or failed. Twenty eight patients in each group completed the study and their average age was around 5 years. Children receiving the antibiotic were more likely to be cured (50% vs. 14%, p=0.01) and less likely to experience treatment failure (14% vs. 68%, p<0.001) than children receiving placebo. Similar to other studies, there were more side effects in the antibiotic treated group compared to the placebo treatment (44% vs. 14% of children, p=0.014). In another randomized, controlled study in patients 1-15 years of age with clinical and radiographic signs and symptoms of ARS, patients received either a cephalosporin (cefditoren 8-12 mg/kg daily) or amoxicillin/ clavulanate (80-90 mg/kg amoxicillin daily) for 14 days (481). The results show comparable, not statistically different, rates of improvement at 14 days: 78.8% for cefditoren and 84.7% for amoxicillin/clavulanate. The median time to improvement was 3 days in both groups and the rate of diarrhoea was significantly higher in the patients treated with amoxicillin/clavulanate (18%) compared to those treated with cefditoren (4.5%).
Most episodes of ARS are self-limited and will resolve spontaneously.
3.6.7.1. Antibiotics
Antibiotics are the most frequently used therapeutic agents in ARS (Table 3.6.1). Published trials in children and adults were reviewed in a recent meta-analysis of randomized controlled trials evaluating antibiotic treatment for ARS in which 3 of the 17 evaluated studies were performed in the paediatric age group (345). In total, 3291 outpatients (2915 adults and 376 children) were treated in the trials included in the meta-analysis. The diagnosis of ARS in the trials was based on clinical criteria in most studies and radiologic and other laboratory criteria in the rest. In most studies, inclusion of patients with viral upper respiratory tract infections was avoided by enrolling patients whose symptoms were of more than 7-10 days duration. The results suggest that, compared with placebo, antibiotics were associated with a higher rate of cure or improvement within 7-15 days with the rate of resolution of symptoms being faster with antibiotics in most randomized controlled trials. The overall positive effect in favour of antibiotics was significant but modest. No difference in cure was found when a subgroup analysis was performed for age. A more recent randomized, placebo-controlled trial not included in the meta-analysis evaluated the efficacy of amoxicillin (90 mg/kg) with potassium clavulanate (6.4 mg/kg) or placebo in children 1-10 years of age with a clinical presentation compatible with bacterial ARS (persistent symptoms, acutely worsening symptoms or severe symptoms) (351). Symptom scores were obtained at multiple time points and the children were evaluated at day 14 from onset of treatment and their condition rated as cured, improved, or failed. Twenty eight patients in each group completed the study and their average age was around 5 years. Children receiving the antibiotic were more likely to be cured (50% vs. 14%, p=0.01) and less likely to experience treatment failure (14% vs. 68%, p<0.001) than children receiving placebo. Similar to other studies, there were more side effects in the antibiotic treated group compared to the placebo treatment (44% vs. 14% of children, p=0.014). In another randomized, controlled study in patients 1-15 years of age with clinical and radiographic signs and symptoms of ARS, patients received either a cephalosporin (cefditoren 8-12 mg/kg daily) or amoxicillin/ clavulanate (80-90 mg/kg amoxicillin daily) for 14 days (481). The results show comparable, not statistically different, rates of improvement at 14 days: 78.8% for cefditoren and 84.7% for amoxicillin/clavulanate. The median time to improvement was 3 days in both groups and the rate of diarrhoea was significantly higher in the patients treated with amoxicillin/clavulanate (18%) compared to those treated with cefditoren (4.5%).
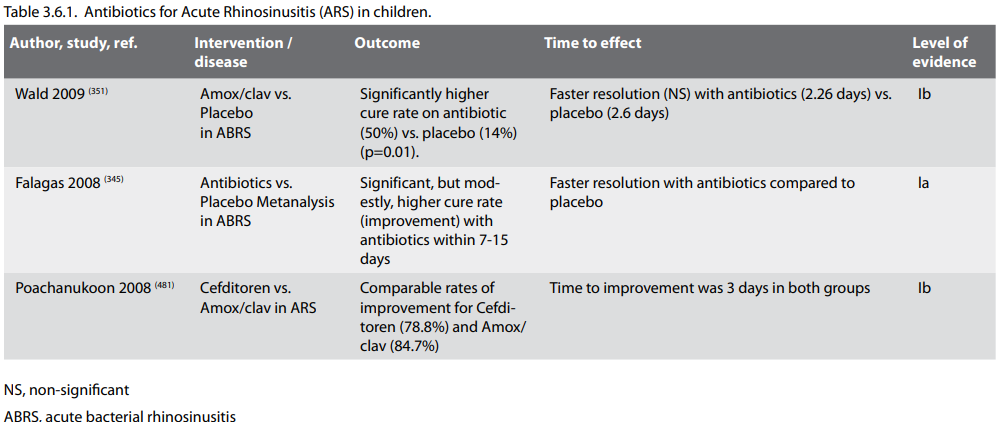
Most of these studies could be criticized for potentially
including patients with ongoing viral URIs and selecting
patients on the basis of clinical symptoms and exam only,
without radiologic documentation. The results, however, suggest
that most cases of uncomplicated acute sinusitis will improve
irrespective of treatment used but will do so faster, and will
have a higher chance of improvement, if given antibiotics. Based
on this evidence, it would seem reasonable to recommend only
symptomatic treatment for uncomplicated episodes of ARS in
children. Antibiotic therapy would be reserved to children with
complications, or concomitant disease that could be exacerbated
by ARS (asthma, chronic bronchitis). In some situations,
children with purulent rhinorrhoea are prevented from staying in
day-care and thus have created problems for working parents.
Whether an acceleration of improvement of the symptoms with
antibiotics in these children is worth the increased risk of
antimicrobial resistance remains to be determined. (Strength of
recommendation: A).
Antibiotic therapy seems to accelerate resolution of ARS in children but whether an acceleration of improvement of the symptoms with antibiotics in these children is worth the increased risk of antimicrobial resistance remains to be determined.
When considering antibiotic choices, uncomplicated ARS in a child who has not received multiple previous courses of antibiotics can still be treated with amoxicillin (40 mg/ kg/day or 80 mg/kg/day). Other reasonable and safe choices are amoxicillin/clavulanate and cephalosporins that provide good coverage of typical organisms, especially those producing β-lactamase (8). If hypersensitivity to any of the above antimicrobials is suspected, alternative choices include trimethoprim/sulfamethoxasole, azithromycin, or clarithromycin. Clindamycin is useful if anaerobic organisms are suspected but provides no coverage against gram-negative organisms.
3.6.7.2. Intranasal Steroids
Intranasal steroids might have a beneficial ancillary role in the treatment of ARS.
In a paediatric trial, 89 children with ARS received amoxicillinclavulanate and were randomized to receive either budesonide or placebo nasal sprays for 3 weeks (307). There were significant improvements in the scores of cough and nasal discharge at the end of the second week in the steroid group compared to placebo suggesting a benefit of adding intranasal steroids to antibiotics in the treatment of ARS. Several trials in mixed adult and paediatric populations (usually 12-14 years and older) have demonstrated similar benefits of using an intranasal steroid along with an antibiotic for the treatment of ARS (306, 482). Therefore there is reasonable evidence to support the addition of an intranasal steroid to antibiotics in the treatment of ARS (Strength of recommendation: A). Finally, in a randomized, placebo controlled, trial in patients older than 12 years with ARS, mometasone 200 mcg twice daily (twice the allergic rhinitis dose) was more effective in controlling symptoms than placebo and amoxicillin (310). Thus, there is also some evidence that a high dose of intranasal steroids in older children might be effective as monotherapy for ARS. However, generalizing to younger children is not justified in the absence of more studies.
3.6.7.3. Ancillary therapy
Ancillary therapies have not been shown to be helpful in ARS.
A systematic review of the literature was undertaken to evaluate the efficacy of decongestants (oral or intranasal), antihistamines, and nasal irrigation in children with clinically diagnosed acute sinusitis (328). Randomized controlled trials (RCTs) or quasi-RCTs that evaluated children 0-18 years of age with ARS defined as 10-30 days of rhinorrhoea, congestion or daytime cough were included. Of 402 articles reviewed 44 references were retrieved and were all excluded because they did not satisfy the set criteria. The authors conclude that there is no evidence to determine whether the use of the above mentioned agents is efficacious in children with ARS. In a more recent publication, erdosteine, a mucolytic agent, was investigated in a randomized, placebo controlled trial (335). Eighty one patients completed the study and their average age was 8.5 years and they all had symptoms consistent with ARS. They were randomized to receive either erdosteine or placebo for 14 days and their symptoms recorded. Both treatment groups had an improvement in symptoms on day 14 but there were not statistically significant differences between the active and placebo groups. Therefore, there is really no good evidence to support the use of ancillary therapies in the treatment of ARS in children (Table 3.6.2) (Strength of recommendation: A-, negative).
Antibiotic therapy seems to accelerate resolution of ARS in children but whether an acceleration of improvement of the symptoms with antibiotics in these children is worth the increased risk of antimicrobial resistance remains to be determined.
When considering antibiotic choices, uncomplicated ARS in a child who has not received multiple previous courses of antibiotics can still be treated with amoxicillin (40 mg/ kg/day or 80 mg/kg/day). Other reasonable and safe choices are amoxicillin/clavulanate and cephalosporins that provide good coverage of typical organisms, especially those producing β-lactamase (8). If hypersensitivity to any of the above antimicrobials is suspected, alternative choices include trimethoprim/sulfamethoxasole, azithromycin, or clarithromycin. Clindamycin is useful if anaerobic organisms are suspected but provides no coverage against gram-negative organisms.
3.6.7.2. Intranasal Steroids
Intranasal steroids might have a beneficial ancillary role in the treatment of ARS.
In a paediatric trial, 89 children with ARS received amoxicillinclavulanate and were randomized to receive either budesonide or placebo nasal sprays for 3 weeks (307). There were significant improvements in the scores of cough and nasal discharge at the end of the second week in the steroid group compared to placebo suggesting a benefit of adding intranasal steroids to antibiotics in the treatment of ARS. Several trials in mixed adult and paediatric populations (usually 12-14 years and older) have demonstrated similar benefits of using an intranasal steroid along with an antibiotic for the treatment of ARS (306, 482). Therefore there is reasonable evidence to support the addition of an intranasal steroid to antibiotics in the treatment of ARS (Strength of recommendation: A). Finally, in a randomized, placebo controlled, trial in patients older than 12 years with ARS, mometasone 200 mcg twice daily (twice the allergic rhinitis dose) was more effective in controlling symptoms than placebo and amoxicillin (310). Thus, there is also some evidence that a high dose of intranasal steroids in older children might be effective as monotherapy for ARS. However, generalizing to younger children is not justified in the absence of more studies.
3.6.7.3. Ancillary therapy
Ancillary therapies have not been shown to be helpful in ARS.
A systematic review of the literature was undertaken to evaluate the efficacy of decongestants (oral or intranasal), antihistamines, and nasal irrigation in children with clinically diagnosed acute sinusitis (328). Randomized controlled trials (RCTs) or quasi-RCTs that evaluated children 0-18 years of age with ARS defined as 10-30 days of rhinorrhoea, congestion or daytime cough were included. Of 402 articles reviewed 44 references were retrieved and were all excluded because they did not satisfy the set criteria. The authors conclude that there is no evidence to determine whether the use of the above mentioned agents is efficacious in children with ARS. In a more recent publication, erdosteine, a mucolytic agent, was investigated in a randomized, placebo controlled trial (335). Eighty one patients completed the study and their average age was 8.5 years and they all had symptoms consistent with ARS. They were randomized to receive either erdosteine or placebo for 14 days and their symptoms recorded. Both treatment groups had an improvement in symptoms on day 14 but there were not statistically significant differences between the active and placebo groups. Therefore, there is really no good evidence to support the use of ancillary therapies in the treatment of ARS in children (Table 3.6.2) (Strength of recommendation: A-, negative).