Burden of Rhinosinusitis
7.1. Quality of Life measurements in the diagnosis and outcome measurement of CRS with and without NP
7.1.1. Introduction
There is now growing acceptance that patients' views are essential in the delivery of high quality care. In addition to enquiries regarding overall severity of CRS symptoms using the VAS, individual symptom severity may be recorded, either using a VAS, or using validated symptom-based questionnaires. Patient Reported Outcome Measures (PROMs) are measures of health-related quality of life (HRQOL) that are self-rated and reported directly by patient. They usually refer to a single time point or clearly defined preceding period, thus 'outcome' measure in this setting is a misnomer. The impact of chronic disease or medical care can be determined by comparing repeated measures of patient's self reported health status. As symptoms drive a patient to seek medical care, measurement of the impact of these symptoms will better reflect the efficacy of treatment from the patient's perspective than a clinician-rated outcome.
Quality of life is measured using one of a growing number of 'instruments'; typically these are questionnaires, but in some cases visual scales or grading systems can be used. These allow quantitative assessment of otherwise subjective results. The questionnaires usually require the patient to rate the impact of their disease across a number of specified 'domains' or areas of interest. Individual questions are scored according to severity or impact of disease, and then scores are combined to produce an overall score. Some PROMs have been developed for particular conditions or treatments (disease-specific) while others are designed for use in all patient groups or healthy individuals and measure the patient's perception of their general health (generic measures).
Generic PROMS allow comparison between conditions or treatments, and therefore can be used to determine the impact of different diseases on patient groups, the relative cost utility of different interventions and to inform commissioning decisions. However, they are often lack sensitivity to detect small but important changes in disease specific QOL. There are now several different rhinosinusitis-specific instruments available, differing in terms of aims of use, number of items, setting and ease of use. In addition, the choice of instrument will depend upon the aim of outcome measurement.
HRQOL is defined across two main domains; psychosocial and physical functioning, and the impact that disease has on this as rated by the patient. Therefore an instrument that measures HRQOL should include items pertaining to both domains. In addition, there are a number of validated questionnaires that include only physical functioning as defined by disease specific symptoms only, without a psychosocial domain, and some measuring cost-effectiveness. These have been included for completeness.
7.1.2. Assessment of Instruments
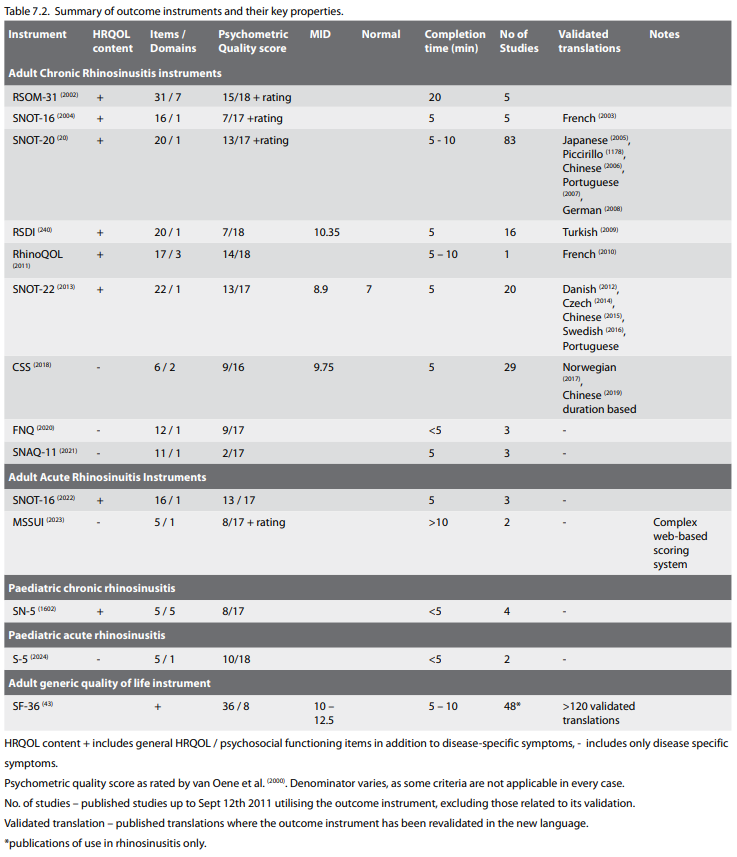
All instruments must have a published psychometric validation in the appropriate setting (e.g. for inclusion under ARS instruments, the instrument must be validated in a group of patients with ARS) to be considered for inclusion – several questionnaires were excluded on this basis. Further quality assessment was undertaken using the scoring system described by van Oene (2000) et al. in a systematic review of outcome tools undertaken in 2007. This excellent scoring system comprehensively captures aspects of instrument validity, including construction of the questionnaire, description of the items and domains, feasibility and respondent burden, size of validation study and reliability in terms of internal consistency, test-retest reliability, content, convergent and discriminant validity, responsiveness, and calculation of the minimally important difference.
The time to complete an instrument will determine it's practical applications, and the times presented were taken from the validation papers where published, and by trialling the tools directly.
Finally, the number of published studies utilising each instrument (excluding those reporting the validation of the instrument), and the number of validated translations are presented. If an instrument is to be translated, it must be done in both a forward and backward direction to ensure the original meaning of the items is retained, and then must be revalidated to ensure it has the same psychometric properties.
7.1.3. Results
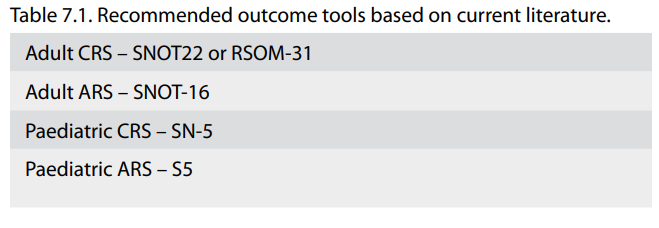
The identified outcome instruments and key properties are summarised in Table 7.1.
7.1.1. Introduction
There is now growing acceptance that patients' views are essential in the delivery of high quality care. In addition to enquiries regarding overall severity of CRS symptoms using the VAS, individual symptom severity may be recorded, either using a VAS, or using validated symptom-based questionnaires. Patient Reported Outcome Measures (PROMs) are measures of health-related quality of life (HRQOL) that are self-rated and reported directly by patient. They usually refer to a single time point or clearly defined preceding period, thus 'outcome' measure in this setting is a misnomer. The impact of chronic disease or medical care can be determined by comparing repeated measures of patient's self reported health status. As symptoms drive a patient to seek medical care, measurement of the impact of these symptoms will better reflect the efficacy of treatment from the patient's perspective than a clinician-rated outcome.
Quality of life is measured using one of a growing number of 'instruments'; typically these are questionnaires, but in some cases visual scales or grading systems can be used. These allow quantitative assessment of otherwise subjective results. The questionnaires usually require the patient to rate the impact of their disease across a number of specified 'domains' or areas of interest. Individual questions are scored according to severity or impact of disease, and then scores are combined to produce an overall score. Some PROMs have been developed for particular conditions or treatments (disease-specific) while others are designed for use in all patient groups or healthy individuals and measure the patient's perception of their general health (generic measures).
Generic PROMS allow comparison between conditions or treatments, and therefore can be used to determine the impact of different diseases on patient groups, the relative cost utility of different interventions and to inform commissioning decisions. However, they are often lack sensitivity to detect small but important changes in disease specific QOL. There are now several different rhinosinusitis-specific instruments available, differing in terms of aims of use, number of items, setting and ease of use. In addition, the choice of instrument will depend upon the aim of outcome measurement.
HRQOL is defined across two main domains; psychosocial and physical functioning, and the impact that disease has on this as rated by the patient. Therefore an instrument that measures HRQOL should include items pertaining to both domains. In addition, there are a number of validated questionnaires that include only physical functioning as defined by disease specific symptoms only, without a psychosocial domain, and some measuring cost-effectiveness. These have been included for completeness.
7.1.2. Assessment of Instruments
All instruments must have a published psychometric validation in the appropriate setting (e.g. for inclusion under ARS instruments, the instrument must be validated in a group of patients with ARS) to be considered for inclusion – several questionnaires were excluded on this basis. Further quality assessment was undertaken using the scoring system described by van Oene (2000) et al. in a systematic review of outcome tools undertaken in 2007. This excellent scoring system comprehensively captures aspects of instrument validity, including construction of the questionnaire, description of the items and domains, feasibility and respondent burden, size of validation study and reliability in terms of internal consistency, test-retest reliability, content, convergent and discriminant validity, responsiveness, and calculation of the minimally important difference.
The time to complete an instrument will determine it's practical applications, and the times presented were taken from the validation papers where published, and by trialling the tools directly.
Finally, the number of published studies utilising each instrument (excluding those reporting the validation of the instrument), and the number of validated translations are presented. If an instrument is to be translated, it must be done in both a forward and backward direction to ensure the original meaning of the items is retained, and then must be revalidated to ensure it has the same psychometric properties.
7.1.3. Results
The identified outcome instruments and key properties are summarised in Table 7.1.
There are several validated tools available for use in CRS in the adult population. The predominant differences between the tools are the number of items. There is a direct relationship between the number of items and the respondent burden, and this should be considered when selecting an instrument for use. 2 instruments (SNOT-20 and SNOT-22) including general HRQOL items rate highly in terms of psychometric quality, and have a significant volume of published studies where the tools have been used, to provide comparative data. However, the SNOT-20 lacks items pertaining to nasal obstruction and reduced sense of smell, and as they are essential for the diagnosis of CRS, we do not feel the SNOT-20 to have adequate content validity to recommend use. The CSS contains only disease specific items but is widely used in the literature.
There are fewer tools available for adult ARS, and for both paediatric CRS and ARS.
Although there are many generic HRQOL instruments, the SF-36 has been extensively used both in rhinosinusitis and other chronic diseases, and provides a wealth of normative and comparative data. The short form 36 (SF-36) is a multipurpose, 36-item survey that measures eight domains of health: physical functioning, role limitations due to physical health, bodily pain, general health perceptions, vitality, social functioning, role limitations due to emotional problems, and mental health. It has been widely used in many medical conditions and over 5000 publications, with normative values available for the general population (SF website). It has been used to measure both the impact of CRS on quality of life, and to assess the outcome of treatment (15, 2001).
Health related quality of life can be measured using a large number of disease-specific or global patient-rated outcome measures
7.1.4. Impact of ARS on quality of life
While the socio-economic burden of acute rhinosinusitis has been measured in terms of medical consultation, medication usage and absenteeism, there is a relative paucity in the literature regarding the impact of acute sinusitis on quality of life. As episodes are by definition short-lived, impairment in quality of life should also be transient, returning to baseline levels after recovery. In addition, due to variation in the definition used in studies, most groups described in clinical trials are a heterogeneous group of patient with a viral 'common cold' and acute bacterial sinusitis.
There is one disease-specific patient rated outcome measure validated for use in ARS. Using the SNOT-16 (2022) in a group of 166 patients, the mean scores declined steadily from 1.71 (SD 0.5 at onset of illness) to 1.13 (SD0.54) at day 3, 0.74 (SD 0.5) at day 7 and falling to 0.49 (SD0.44) by day 10. In terms of comparison with CRS, and normal patients one study reports the use of the SF-36, with significant differences between all groups (p<0.001), with patients with ARS having poorer HRQOL (mean score 60.8) than healthy individuals (51.8), but less reduction than those with CRS (75.5) (2025). In terms of specific symptoms, a recent survey based study in France asked physicians to report symptom frequency and severity prospectively on patients with a diagnosis of acute maxillary sinusitis (228). The most common presenting signs and symptoms were moderate-tosevere nasal obstruction (80.4%), pain on sinus palpitation (76.8%), facial pain (74.5%), rhinorrhoea (70.4%), and headache (63.6%). Symptoms were indicated as having a moderate to very significant effect on quality of life areas including activities of daily living (71.6% of patients), leisure (63.1%), and professional/ school activities (59.2%). In a prospective randomized, doubleblind, placebo-controlled trial (311), comparing the effect of antibiotics and topical steroids, the most severe symptoms were post-nasal discharge, need to blow nose, runny nose and waking up tired, using the SNOT-20 to assess symptom severity (which therefore does not capture nasal obstruction or anosmia). This study demonstrated significant improvement in health related quality of life from baseline to the end of the trial period at day 15, with mometasone producing a significantly greater improvement in the SNOT-20 mean total score than that seen with placebo (p = 0.047).
A number of disease-specific and global patient-rated outcome measures have been used to demonstrate significant impairment in HRQOL in both ARS and CRS
There are fewer tools available for adult ARS, and for both paediatric CRS and ARS.
Although there are many generic HRQOL instruments, the SF-36 has been extensively used both in rhinosinusitis and other chronic diseases, and provides a wealth of normative and comparative data. The short form 36 (SF-36) is a multipurpose, 36-item survey that measures eight domains of health: physical functioning, role limitations due to physical health, bodily pain, general health perceptions, vitality, social functioning, role limitations due to emotional problems, and mental health. It has been widely used in many medical conditions and over 5000 publications, with normative values available for the general population (SF website). It has been used to measure both the impact of CRS on quality of life, and to assess the outcome of treatment (15, 2001).
Health related quality of life can be measured using a large number of disease-specific or global patient-rated outcome measures
7.1.4. Impact of ARS on quality of life
While the socio-economic burden of acute rhinosinusitis has been measured in terms of medical consultation, medication usage and absenteeism, there is a relative paucity in the literature regarding the impact of acute sinusitis on quality of life. As episodes are by definition short-lived, impairment in quality of life should also be transient, returning to baseline levels after recovery. In addition, due to variation in the definition used in studies, most groups described in clinical trials are a heterogeneous group of patient with a viral 'common cold' and acute bacterial sinusitis.
There is one disease-specific patient rated outcome measure validated for use in ARS. Using the SNOT-16 (2022) in a group of 166 patients, the mean scores declined steadily from 1.71 (SD 0.5 at onset of illness) to 1.13 (SD0.54) at day 3, 0.74 (SD 0.5) at day 7 and falling to 0.49 (SD0.44) by day 10. In terms of comparison with CRS, and normal patients one study reports the use of the SF-36, with significant differences between all groups (p<0.001), with patients with ARS having poorer HRQOL (mean score 60.8) than healthy individuals (51.8), but less reduction than those with CRS (75.5) (2025). In terms of specific symptoms, a recent survey based study in France asked physicians to report symptom frequency and severity prospectively on patients with a diagnosis of acute maxillary sinusitis (228). The most common presenting signs and symptoms were moderate-tosevere nasal obstruction (80.4%), pain on sinus palpitation (76.8%), facial pain (74.5%), rhinorrhoea (70.4%), and headache (63.6%). Symptoms were indicated as having a moderate to very significant effect on quality of life areas including activities of daily living (71.6% of patients), leisure (63.1%), and professional/ school activities (59.2%). In a prospective randomized, doubleblind, placebo-controlled trial (311), comparing the effect of antibiotics and topical steroids, the most severe symptoms were post-nasal discharge, need to blow nose, runny nose and waking up tired, using the SNOT-20 to assess symptom severity (which therefore does not capture nasal obstruction or anosmia). This study demonstrated significant improvement in health related quality of life from baseline to the end of the trial period at day 15, with mometasone producing a significantly greater improvement in the SNOT-20 mean total score than that seen with placebo (p = 0.047).
A number of disease-specific and global patient-rated outcome measures have been used to demonstrate significant impairment in HRQOL in both ARS and CRS
7.1.5. Impact of CRS on quality of life
Using the SF-36, chronic rhinosinusitis has been shown to have a negative impact on several aspects of quality of life, and has a greater impact on social functioning the chronic heart failure, angina or back pain (2001). Published studies report scores below the normal population in 5 – 7 of the SF-36 domains (2001, 2026, 2027). The SNOT-22 was shown to have a median value of 7 in healthy volunteers, compared to a mean pre-operative SNOT-22 score of 42.0 (95% CI = 41.2-42.7) in a cohort of 3,128 patients undergoing surgery for CRS (2028). Several studies have shown that CRSwNP tend to report better QOL than those with CRSsNP despite worse CT and endoscopy scores (1885).
Improvement following both medical and surgical intervention has been demonstrated in CRS using PROMS
Quality of life measures may also be used to evaluate changes over time following either medical or surgical intervention. In the large cohort study above, the mean SNOT-22 score for all patients was 28.2 (standard deviation [SD] = 22.4) at 5 years after surgery (1758). This was remarkably similar to the results observed at 3 months (25.5), 12 months (27.7), and 36 months (27.7), and represents a 14-point improvement over the baseline score (ES 0.8SD).
Chester et al. (2029) undertook a systematic review of the literature reporting symptomatic outcome following FESS. The metaanalysis of 21 of 289 identified FESS studies was conducted for each symptom separately with the standardized difference between the preoperative and postoperative severity scores as the effect size (ES). ESS symptom outcomes were reported using various symptom scoring systems and more than 18 survey instruments. A total of 2070 patients with CRS were studied a mean of 13.9 months after ESS. All symptoms demonstrated improvement compared with their respective preoperative severity scores by an overall ES of 1.19 (95% confidence interval, 0.96 to 1.41; I (2) = 81.7%) using the random-effects model. Nasal obstruction (ES, 1.73) improved the most, with facial pain (ES, 1.13) and postnasal discharge (ES, 1.19) demonstrating moderate improvements. Hyposmia (ES, 0.97) and headache (ES, 0.98) improved the least. When individual symptom scores were pooled by meta-analysis, most major CRS symptoms improved to a similar degree following surgery, with an overall effect size of 1.19 (95% confidence interval, 0.96-1.41; I (2) = 82%). Fatigue and bodily pain were more severe than general population normative values and improved following ESS by an effect size of approximately 0.5 SD, a change usually regarded as a minimally important clinical difference.
The impact on different treatment modalities is considered in more detail in each relevant section.
7.2. Direct Costs
7.2.1. Direct costs of chronic rhinosinusitis
Chronic rhinosinusitis (CRS) (with and without polyps) is a frequent pathology with a high impact on quality of life. The research concerning the socioeconomic impact of the disease is limited. Ray et al estimated, already in 1999 the total direct cost in the US at 5,78 billion dollars per year (2030).
In US the total cost of treating a patient with CRS was $2609 per year; in Europe the direct costs of a patient treated in a university hospital for severe chronic rhinosinusitis was $1861/year
In 2002, Murphy et al (2031) examined the direct costs of a patient with a diagnosis of CRS. These patients seemed to make 43% more outpatient and 25% more urgent care visits than a patient without CRS. CRS patients filed 43% more subscriptions, but had fewer hospital stays. The total cost of treating a patient with CRS was $2609 per year; this is 6% more than the average adult. In Europe only one study was found, in the Netherlands, executed by van Agthoven et al. Here the direct costs of a patient treated in a university hospital for severe chronic rhinosinusitis was $1861/year (2032).
In addition to these findings, also mentioned in EPOS2007, a search was made through recent English literature 2007-December 2011. The studies discussed are all carried out by N. Bhattacharyya and his team. The studies are well performed and concern a big amount of data, but are limited to USA patients. There are no recent studies carried out in Europe. In March 2009 Bhattacharyya (2033) published the assessment of the additional disease burden of nasal polyps in CRS. A series of patients were recruited from their centre. Patients were included according to the Rhinosinusitis symptom inventory (Task force on Rhinosinusitis criteria) and by findings with nasal endoscopy and on CT (Lund MacKay score). Three groups were composed: one with CRS without nasal polyps (CRSsNP), a second group with CRS with nasal polyps (CRSwNP) and a third with CRS with recurrent nasal polyps after surgery.
The groups with and without nasal polyps show a clear difference in symptom phenotype, but this did not translate into a difference in expenditures for physician's visits and medication costs between the first 2 groups. There was no statistically significant difference. However there was a difference in total medication costs for the last group with recurrent polyps after surgery with a higher cost for this group of $ 865.50 compared to the $ 569.60 for group 1 and $ 564.50 for group 2. In July 2009 a contemporary assessment of the disease burden of sinusitis from Bhattacharyya (37) was published. Here data were extracted from the National Health interview survey over a 10-year period of 1997-2006. One year disease prevalences show that one quarter (22.7%) of patients with CRS visited an emergency department, one third (33.6%) saw a medical specialist, more than half (55.8%) spent $500 or more per year on health care. Health care spending was significantly greater in sinusitis than that of other chronic diseases as ulcer disease, acute asthma and hay fever.
National health care costs in the US remain very high for CRS, at an estimated 8.6 billion dollar per year (2034). Factors contributing to a high economic impact of this condition are: the high disease prevalence (10 to 14% of the population would be affected), it is a chronic condition with no universal cure, there are frequent exacerbations of symptoms prompting acute treatments in addition to the chronic ones already in place, there is a high quality of life-impact, a generally incomplete symptom control leading patients to seek additional therapies to achieve relief and it is difficult to accurately diagnose the condition without radiologic or diagnostic procedures (2035).
The highest costs were made by the group with recurrent polyps after surgery
In 2011 Bhattacharyya (2034) calculated the incremental health care utilization and expenditure for CRS in the United States. Patient data were extracted from the Medical Expenditure Panel Survey. With the incremental expenditure methodology, expenditures are measured attributable particular to CRS, there is adjusted for differences in variables that are having an impact on expenditures, like age, gender, insurance status etc. For the expenditures next components are taken into consideration: office-based health care expenditures, prescription expenditures and patients' self-expenditures for prescription medications. For utilization of health care, data show that CRS patients incurred ±3, 5 additional office visits and 5,5 additional prescription fills compared to patients without CRS. This extra utilization of healthcare evokes higher expenditures; a CRS patient would have a substantial incremental increase of total health care expenditure of $772 (±$300) consisting of $346(±$130) for office-based expenditures, $397(±$88) for prescription expenditures and $90(±$24) for self-expenditures. Bhattacharyya et al. (2035) reported the costs pre- and postoperative to Endoscopic Sinus Surgery (ESS). Data come from the Market Scan Commercial Claims and Encounters Database from 2003 to 2008. Numerous studies have shown the effectiveness of surgery in improving quality of life in CRS patients, but the effect of surgery on expenditures was not clarified. Patients were included if 2 CRS-related diagnoses were retrieved, confirmed by either CT-scan or endoscopy. Likely this might cause a selection of more severe cases. Patients with nasal polyps were excluded from this study. All sinus-related health care utilization costs were rolled up in the study (medication, operation costs, office visits, diagnostic assessment with radiology and endoscopy). Results show that in the year prior to ESS costs run op to $2,449 ($2,341-$2,556) with a clear increase in the last 6 months before surgery; the first semester accounts for $361 and the last semester for $1,965. This is due to an augmentation in office visits, diagnostic investigations and medication use. The augmentation in prescription medication is for the greatest part due to a higher antibiotic use; from $75 in the first to $225 in the second semester.
The ESS-procedure and the 45-day post procedure period count for $7,726 ($7,554 – $7,898). In the first year following ESS, costs drop by $885 to an average of $1,564 per year. In the second year post procedure they drop an additional $446 to $1,118 per year. This decrease was mostly due to a lower amount of doctor visits, there was only a minor change in the costs of anti-inflammatory medication. Important to mention is that the costs in the 4th semester postoperative remain higher than in the first semester preoperative, possibly inflammation does not return to premorbid levels.
Health care spending was significantly greater in sinusitis than in other chronic diseases such as ulcer disease, acute asthma and hay fever
From above studies we see that the direct costs of CRS are quite high (average $772), also compared to other chronic diseases. In the year prior to surgery the disease burden augments and also causes a strong increase in costs ($2,449/patient/year).
Endoscopic sinus surgery is expensive ($7,726 for procedure and 45-day follow-up), but causes a drop of costs in the 2 years post operative (average $1,564 in year 1, average $1,118 in year 2). The important clinical difference in CRS with and without polyps only causes a difference in medication costs for the group with recurrence of polyps after surgery; probably this group has a higher disease severity.
Endoscopic sinus surgery is expensive, but causes a drop in costs for the 2 post-operative years
Above data is all from the same principal investigator, which shows that there is little interest in the economic burden of CRS. There were no recent European data available, although many important questions remain unanswered, like: What would be the personal costs and the health insurance costs in European countries with different health care systems than in the US? Which link is there between disease severity and costs?
7.2.2. Direct costs of acute rhinosinusitis
Besides the pathology of chronic rhinosinusitis, also acute rhinosinusitis can be an economic burden. Anand estimated in 2004 that there are approximately 20 million cases of acute bacterial rhinosinusitis yearly in the United States (2036). One in 3,000 adults would suffer from a recurrent acute rhinosinusitis (43). This entity was in the study of Bhattacharyya defined as at least 4 claims of sinusitis in 12 months, with antibiotic prescription; this with a relative paucity of symptoms at baseline between episodes. Considering this definition, there might be an overlap with the diagnosis of CRS. This patient group has an average of 5,6 health care visits/year, 9,4 prescriptions filled (40% antibiotic). Only 20% of patients had either a nasal endoscopy or CT scan annually. This probably means that only a small part sees an ENT-specialist for his complaints.
The total direct health care cost of recurrent acute rhinosinusitis would be an average of $1,091/year: $210 to antibiotics, $452 to other sinus-related prescriptions (relatively large cost due to leukotriene inhibitors who are not generically available), $47 to imaging and $382 to other visit costs.
Patients with recurrent acute rhinosinusitis have an average direct health care cost of $1,091/year in average (US)
A study in Taiwan showed that acute nasopharyngitis and acute upper respiratory tract infections were the 2 diseases with the highest number of outpatient department visits (2037). The drug expenditure for acute respiratory infections accounted for 6% of total drug expenditure. Only 42,8% of drugs for these illnesses was described as suitable for patients' self-care. Sinusitis cannot only cause direct costs on it's own, but especially as comorbidity with asthma it is known to augment disease burden. Bhattacharyya et al. studied in 2009 the additional disease burden from hay fever and sinusitis accompanying asthma (2038). This showed that there were more emergency room visits from patients with asthma and sinusitis, than of those with only asthma or a comorbidity of hay fever. The total health care visits and the household healthcare expenditures are higher for this group of patients.
Total health care costs and the household healthcare expenditures are higher for patients with sinusitis and asthma
The above studies show that also acute sinusitis is an important pathology to consider economically. Because of the high prevalence, the risk of recurrence and the augmentation of disease burden to chronic conditions as asthma. Literature does not give an answer to the question how much one episode of acute sinusitis would cost; this can be an objective for future investigations.
Using the SF-36, chronic rhinosinusitis has been shown to have a negative impact on several aspects of quality of life, and has a greater impact on social functioning the chronic heart failure, angina or back pain (2001). Published studies report scores below the normal population in 5 – 7 of the SF-36 domains (2001, 2026, 2027). The SNOT-22 was shown to have a median value of 7 in healthy volunteers, compared to a mean pre-operative SNOT-22 score of 42.0 (95% CI = 41.2-42.7) in a cohort of 3,128 patients undergoing surgery for CRS (2028). Several studies have shown that CRSwNP tend to report better QOL than those with CRSsNP despite worse CT and endoscopy scores (1885).
Improvement following both medical and surgical intervention has been demonstrated in CRS using PROMS
Quality of life measures may also be used to evaluate changes over time following either medical or surgical intervention. In the large cohort study above, the mean SNOT-22 score for all patients was 28.2 (standard deviation [SD] = 22.4) at 5 years after surgery (1758). This was remarkably similar to the results observed at 3 months (25.5), 12 months (27.7), and 36 months (27.7), and represents a 14-point improvement over the baseline score (ES 0.8SD).
Chester et al. (2029) undertook a systematic review of the literature reporting symptomatic outcome following FESS. The metaanalysis of 21 of 289 identified FESS studies was conducted for each symptom separately with the standardized difference between the preoperative and postoperative severity scores as the effect size (ES). ESS symptom outcomes were reported using various symptom scoring systems and more than 18 survey instruments. A total of 2070 patients with CRS were studied a mean of 13.9 months after ESS. All symptoms demonstrated improvement compared with their respective preoperative severity scores by an overall ES of 1.19 (95% confidence interval, 0.96 to 1.41; I (2) = 81.7%) using the random-effects model. Nasal obstruction (ES, 1.73) improved the most, with facial pain (ES, 1.13) and postnasal discharge (ES, 1.19) demonstrating moderate improvements. Hyposmia (ES, 0.97) and headache (ES, 0.98) improved the least. When individual symptom scores were pooled by meta-analysis, most major CRS symptoms improved to a similar degree following surgery, with an overall effect size of 1.19 (95% confidence interval, 0.96-1.41; I (2) = 82%). Fatigue and bodily pain were more severe than general population normative values and improved following ESS by an effect size of approximately 0.5 SD, a change usually regarded as a minimally important clinical difference.
The impact on different treatment modalities is considered in more detail in each relevant section.
7.2. Direct Costs
7.2.1. Direct costs of chronic rhinosinusitis
Chronic rhinosinusitis (CRS) (with and without polyps) is a frequent pathology with a high impact on quality of life. The research concerning the socioeconomic impact of the disease is limited. Ray et al estimated, already in 1999 the total direct cost in the US at 5,78 billion dollars per year (2030).
In US the total cost of treating a patient with CRS was $2609 per year; in Europe the direct costs of a patient treated in a university hospital for severe chronic rhinosinusitis was $1861/year
In 2002, Murphy et al (2031) examined the direct costs of a patient with a diagnosis of CRS. These patients seemed to make 43% more outpatient and 25% more urgent care visits than a patient without CRS. CRS patients filed 43% more subscriptions, but had fewer hospital stays. The total cost of treating a patient with CRS was $2609 per year; this is 6% more than the average adult. In Europe only one study was found, in the Netherlands, executed by van Agthoven et al. Here the direct costs of a patient treated in a university hospital for severe chronic rhinosinusitis was $1861/year (2032).
In addition to these findings, also mentioned in EPOS2007, a search was made through recent English literature 2007-December 2011. The studies discussed are all carried out by N. Bhattacharyya and his team. The studies are well performed and concern a big amount of data, but are limited to USA patients. There are no recent studies carried out in Europe. In March 2009 Bhattacharyya (2033) published the assessment of the additional disease burden of nasal polyps in CRS. A series of patients were recruited from their centre. Patients were included according to the Rhinosinusitis symptom inventory (Task force on Rhinosinusitis criteria) and by findings with nasal endoscopy and on CT (Lund MacKay score). Three groups were composed: one with CRS without nasal polyps (CRSsNP), a second group with CRS with nasal polyps (CRSwNP) and a third with CRS with recurrent nasal polyps after surgery.
The groups with and without nasal polyps show a clear difference in symptom phenotype, but this did not translate into a difference in expenditures for physician's visits and medication costs between the first 2 groups. There was no statistically significant difference. However there was a difference in total medication costs for the last group with recurrent polyps after surgery with a higher cost for this group of $ 865.50 compared to the $ 569.60 for group 1 and $ 564.50 for group 2. In July 2009 a contemporary assessment of the disease burden of sinusitis from Bhattacharyya (37) was published. Here data were extracted from the National Health interview survey over a 10-year period of 1997-2006. One year disease prevalences show that one quarter (22.7%) of patients with CRS visited an emergency department, one third (33.6%) saw a medical specialist, more than half (55.8%) spent $500 or more per year on health care. Health care spending was significantly greater in sinusitis than that of other chronic diseases as ulcer disease, acute asthma and hay fever.
National health care costs in the US remain very high for CRS, at an estimated 8.6 billion dollar per year (2034). Factors contributing to a high economic impact of this condition are: the high disease prevalence (10 to 14% of the population would be affected), it is a chronic condition with no universal cure, there are frequent exacerbations of symptoms prompting acute treatments in addition to the chronic ones already in place, there is a high quality of life-impact, a generally incomplete symptom control leading patients to seek additional therapies to achieve relief and it is difficult to accurately diagnose the condition without radiologic or diagnostic procedures (2035).
The highest costs were made by the group with recurrent polyps after surgery
In 2011 Bhattacharyya (2034) calculated the incremental health care utilization and expenditure for CRS in the United States. Patient data were extracted from the Medical Expenditure Panel Survey. With the incremental expenditure methodology, expenditures are measured attributable particular to CRS, there is adjusted for differences in variables that are having an impact on expenditures, like age, gender, insurance status etc. For the expenditures next components are taken into consideration: office-based health care expenditures, prescription expenditures and patients' self-expenditures for prescription medications. For utilization of health care, data show that CRS patients incurred ±3, 5 additional office visits and 5,5 additional prescription fills compared to patients without CRS. This extra utilization of healthcare evokes higher expenditures; a CRS patient would have a substantial incremental increase of total health care expenditure of $772 (±$300) consisting of $346(±$130) for office-based expenditures, $397(±$88) for prescription expenditures and $90(±$24) for self-expenditures. Bhattacharyya et al. (2035) reported the costs pre- and postoperative to Endoscopic Sinus Surgery (ESS). Data come from the Market Scan Commercial Claims and Encounters Database from 2003 to 2008. Numerous studies have shown the effectiveness of surgery in improving quality of life in CRS patients, but the effect of surgery on expenditures was not clarified. Patients were included if 2 CRS-related diagnoses were retrieved, confirmed by either CT-scan or endoscopy. Likely this might cause a selection of more severe cases. Patients with nasal polyps were excluded from this study. All sinus-related health care utilization costs were rolled up in the study (medication, operation costs, office visits, diagnostic assessment with radiology and endoscopy). Results show that in the year prior to ESS costs run op to $2,449 ($2,341-$2,556) with a clear increase in the last 6 months before surgery; the first semester accounts for $361 and the last semester for $1,965. This is due to an augmentation in office visits, diagnostic investigations and medication use. The augmentation in prescription medication is for the greatest part due to a higher antibiotic use; from $75 in the first to $225 in the second semester.
The ESS-procedure and the 45-day post procedure period count for $7,726 ($7,554 – $7,898). In the first year following ESS, costs drop by $885 to an average of $1,564 per year. In the second year post procedure they drop an additional $446 to $1,118 per year. This decrease was mostly due to a lower amount of doctor visits, there was only a minor change in the costs of anti-inflammatory medication. Important to mention is that the costs in the 4th semester postoperative remain higher than in the first semester preoperative, possibly inflammation does not return to premorbid levels.
Health care spending was significantly greater in sinusitis than in other chronic diseases such as ulcer disease, acute asthma and hay fever
From above studies we see that the direct costs of CRS are quite high (average $772), also compared to other chronic diseases. In the year prior to surgery the disease burden augments and also causes a strong increase in costs ($2,449/patient/year).
Endoscopic sinus surgery is expensive ($7,726 for procedure and 45-day follow-up), but causes a drop of costs in the 2 years post operative (average $1,564 in year 1, average $1,118 in year 2). The important clinical difference in CRS with and without polyps only causes a difference in medication costs for the group with recurrence of polyps after surgery; probably this group has a higher disease severity.
Endoscopic sinus surgery is expensive, but causes a drop in costs for the 2 post-operative years
Above data is all from the same principal investigator, which shows that there is little interest in the economic burden of CRS. There were no recent European data available, although many important questions remain unanswered, like: What would be the personal costs and the health insurance costs in European countries with different health care systems than in the US? Which link is there between disease severity and costs?
7.2.2. Direct costs of acute rhinosinusitis
Besides the pathology of chronic rhinosinusitis, also acute rhinosinusitis can be an economic burden. Anand estimated in 2004 that there are approximately 20 million cases of acute bacterial rhinosinusitis yearly in the United States (2036). One in 3,000 adults would suffer from a recurrent acute rhinosinusitis (43). This entity was in the study of Bhattacharyya defined as at least 4 claims of sinusitis in 12 months, with antibiotic prescription; this with a relative paucity of symptoms at baseline between episodes. Considering this definition, there might be an overlap with the diagnosis of CRS. This patient group has an average of 5,6 health care visits/year, 9,4 prescriptions filled (40% antibiotic). Only 20% of patients had either a nasal endoscopy or CT scan annually. This probably means that only a small part sees an ENT-specialist for his complaints.
The total direct health care cost of recurrent acute rhinosinusitis would be an average of $1,091/year: $210 to antibiotics, $452 to other sinus-related prescriptions (relatively large cost due to leukotriene inhibitors who are not generically available), $47 to imaging and $382 to other visit costs.
Patients with recurrent acute rhinosinusitis have an average direct health care cost of $1,091/year in average (US)
A study in Taiwan showed that acute nasopharyngitis and acute upper respiratory tract infections were the 2 diseases with the highest number of outpatient department visits (2037). The drug expenditure for acute respiratory infections accounted for 6% of total drug expenditure. Only 42,8% of drugs for these illnesses was described as suitable for patients' self-care. Sinusitis cannot only cause direct costs on it's own, but especially as comorbidity with asthma it is known to augment disease burden. Bhattacharyya et al. studied in 2009 the additional disease burden from hay fever and sinusitis accompanying asthma (2038). This showed that there were more emergency room visits from patients with asthma and sinusitis, than of those with only asthma or a comorbidity of hay fever. The total health care visits and the household healthcare expenditures are higher for this group of patients.
Total health care costs and the household healthcare expenditures are higher for patients with sinusitis and asthma
The above studies show that also acute sinusitis is an important pathology to consider economically. Because of the high prevalence, the risk of recurrence and the augmentation of disease burden to chronic conditions as asthma. Literature does not give an answer to the question how much one episode of acute sinusitis would cost; this can be an objective for future investigations.
7.3. Indirect Medical Costs
The studies of direct medical costs demonstrate a tremendous social economic burden of Rhinosinusitis. However, the total costs of rhinosinusitis are far greater when the indirect costs are considered. With 85% of patients with Rhinosinusitis of working age (between 18-65 years old) (485), indirect costs such as missed workdays (absenteeism) and decreased productivity at work (presenteeism) significantly add to the economic burden of disease.
Rhinosinusitis is one of the top ten most costly health conditions to US employers
Goetzel et al. (2039) attempted to quantify the indirect costs of rhinosinusitis. Their 2003 study resulted in rhinosinusitis being named one of the top ten most costly health conditions to US employers. A large multi-employer database was used to track insurance claims through employee health insurance, absentee days, and short-term disability claims. Episodes of illness were linked to missed workdays and disability claims, accurately correlating absenteeism to a given disease. In a large sample size (375,000), total healthcare payments per employee per year for sinusitis (acute and chronic) were found to be $60.17, 46% of which came from the cost of absenteeism and disability. These figures approximate the cost to employers, disregarding the cost incurred by other parties, and therefore tremendously underestimate the entire economic burden of the disease.
Indirect costs account for 40% of the total costs of rhinosinusitis
In his 2003 study, Bhattacharyya used patient-completed surveys from 322 patients to estimate the direct and indirect costs of chronic rhinosinusitis (2040). Patients completed a survey assessing symptoms of disease, detailing medication use, and quantifying missed worked days attributable to CRS. The conclusions of the report included that the cost of treating CRS per patient totalled $1,539 per year with forty percent of these costs due to the indirect costs of missed work; the mean number of missed workdays in this sample of 322 patients was 4.8 days (95% CI, 3.4-6.1). The author of the study followed this up in a 2009 report using data from the National Health Interview Survey between 1997 and 2006 encompassing nearly 315,000 individuals and reported that patients with sinusitis missed on average 5.7 days of work per year (37).
A major component of the indirect costs result from absenteeism and presenteeism
The cost burden of absenteeism is enormous, and yet it is only the beginning. The general health status of patients with CRS is poor relative to the normal US population (2001). This decreased quality of life not only leads to absenteeism, but also contributes to the idea of "presenteeism" or decreased productivity when at work. Ray et al. estimated by the 1994 National Health Interview Survey, that missed worked days due to sinusitis was 12.5 million and restricted activity days was 58.7 million days (2030). Economic loss due to presenteeism cannot be easily quantified as it varies from individual to individual, but clearly increases the cost burden of the disease.
Recently Stankiewicz et al. reported on the rates of absenteeism and presenteeism in a population of 71 patients undergoing surgical intervention for chronic rhinosinusitis. Prior to surgery, they report a 6.5% rate of absenteeism (i.e., 6.5% of work time missed) and 36.2% rate of presenteeism (reduction of on-job effectiveness). When combined the rate of absenteeism and presenteeism yielded a 38% work productivity loss in the study population, but no dollar value was placed on this figure (2041). Supporting this, Stull et al. reported that nasal congestion alone resulted in poor sleep, increased fatigue, and daytime sleepiness contributing to decreased work productivity (2042).
Patients with rhinosinusitis miss on average 6 days of work annually due to the disease.
Although incidence rates may be similar to that reported in the U.S. direct and indirect costs would vary widely based upon medical costs, per-capita income and life expectancy. Although in the U.S., chronic rhinosinusitis is estimated to cost as much as $5.78 billion annually in the U.S.2, extrapolation of figures from other studies suggests the possibility of a substantially larger cost. Decreased quality of life in patients suffering from rhinosinusitis results in an average of 4.8 -5.7 missed workdays translating into $600 of decreased productivity annually per patient (2031), contributing to the cost burden of the disease not incorporated into the $5.78 billion. Whatever the precise cost, it is clear that socioeconomic burden of the disease is great and the disease has significant quality of life implications. As such it is therefore imperative that we continue to understand the pathophysiology of the disease and to devise cost effective strategies to provide relief to patients.
Absenteeism and presenteeism for "the Common cold" is also substantial. In a 2002 study, Bramely et al reported each cold experienced by a working adult caused an average of 8.7 lost work hours (2.8 absenteeism hours; 5.9 hours of on-the-job loss/presenteeism), and 1.2 work hours were lost because of attending to children under the age of 13 who were suffering from colds. The study concludes that the economic cost of lost productivity due to the common cold approaches $25 billion, of which $16.6 billion is attributed to on-the-job productivity loss, $8 billion is attributed to absenteeism, and $230 million is attributed to caregiver absenteeism (2043). A more recent study in Sweden by Hellgren et al evaluated the productivity loosed due to the common cold and allergic rhinitis and estimated the economic burden in Sweden alone was €2.7 billion annually. Of the total costs, absenteeism (44%) was the dominant factor, followed by presenteeism (37%) and caregiver absenteeism (19%) (2044).
There are no data on ARS, research is urgently needed.
The studies of direct medical costs demonstrate a tremendous social economic burden of Rhinosinusitis. However, the total costs of rhinosinusitis are far greater when the indirect costs are considered. With 85% of patients with Rhinosinusitis of working age (between 18-65 years old) (485), indirect costs such as missed workdays (absenteeism) and decreased productivity at work (presenteeism) significantly add to the economic burden of disease.
Rhinosinusitis is one of the top ten most costly health conditions to US employers
Goetzel et al. (2039) attempted to quantify the indirect costs of rhinosinusitis. Their 2003 study resulted in rhinosinusitis being named one of the top ten most costly health conditions to US employers. A large multi-employer database was used to track insurance claims through employee health insurance, absentee days, and short-term disability claims. Episodes of illness were linked to missed workdays and disability claims, accurately correlating absenteeism to a given disease. In a large sample size (375,000), total healthcare payments per employee per year for sinusitis (acute and chronic) were found to be $60.17, 46% of which came from the cost of absenteeism and disability. These figures approximate the cost to employers, disregarding the cost incurred by other parties, and therefore tremendously underestimate the entire economic burden of the disease.
Indirect costs account for 40% of the total costs of rhinosinusitis
In his 2003 study, Bhattacharyya used patient-completed surveys from 322 patients to estimate the direct and indirect costs of chronic rhinosinusitis (2040). Patients completed a survey assessing symptoms of disease, detailing medication use, and quantifying missed worked days attributable to CRS. The conclusions of the report included that the cost of treating CRS per patient totalled $1,539 per year with forty percent of these costs due to the indirect costs of missed work; the mean number of missed workdays in this sample of 322 patients was 4.8 days (95% CI, 3.4-6.1). The author of the study followed this up in a 2009 report using data from the National Health Interview Survey between 1997 and 2006 encompassing nearly 315,000 individuals and reported that patients with sinusitis missed on average 5.7 days of work per year (37).
A major component of the indirect costs result from absenteeism and presenteeism
The cost burden of absenteeism is enormous, and yet it is only the beginning. The general health status of patients with CRS is poor relative to the normal US population (2001). This decreased quality of life not only leads to absenteeism, but also contributes to the idea of "presenteeism" or decreased productivity when at work. Ray et al. estimated by the 1994 National Health Interview Survey, that missed worked days due to sinusitis was 12.5 million and restricted activity days was 58.7 million days (2030). Economic loss due to presenteeism cannot be easily quantified as it varies from individual to individual, but clearly increases the cost burden of the disease.
Recently Stankiewicz et al. reported on the rates of absenteeism and presenteeism in a population of 71 patients undergoing surgical intervention for chronic rhinosinusitis. Prior to surgery, they report a 6.5% rate of absenteeism (i.e., 6.5% of work time missed) and 36.2% rate of presenteeism (reduction of on-job effectiveness). When combined the rate of absenteeism and presenteeism yielded a 38% work productivity loss in the study population, but no dollar value was placed on this figure (2041). Supporting this, Stull et al. reported that nasal congestion alone resulted in poor sleep, increased fatigue, and daytime sleepiness contributing to decreased work productivity (2042).
Patients with rhinosinusitis miss on average 6 days of work annually due to the disease.
Although incidence rates may be similar to that reported in the U.S. direct and indirect costs would vary widely based upon medical costs, per-capita income and life expectancy. Although in the U.S., chronic rhinosinusitis is estimated to cost as much as $5.78 billion annually in the U.S.2, extrapolation of figures from other studies suggests the possibility of a substantially larger cost. Decreased quality of life in patients suffering from rhinosinusitis results in an average of 4.8 -5.7 missed workdays translating into $600 of decreased productivity annually per patient (2031), contributing to the cost burden of the disease not incorporated into the $5.78 billion. Whatever the precise cost, it is clear that socioeconomic burden of the disease is great and the disease has significant quality of life implications. As such it is therefore imperative that we continue to understand the pathophysiology of the disease and to devise cost effective strategies to provide relief to patients.
Absenteeism and presenteeism for "the Common cold" is also substantial. In a 2002 study, Bramely et al reported each cold experienced by a working adult caused an average of 8.7 lost work hours (2.8 absenteeism hours; 5.9 hours of on-the-job loss/presenteeism), and 1.2 work hours were lost because of attending to children under the age of 13 who were suffering from colds. The study concludes that the economic cost of lost productivity due to the common cold approaches $25 billion, of which $16.6 billion is attributed to on-the-job productivity loss, $8 billion is attributed to absenteeism, and $230 million is attributed to caregiver absenteeism (2043). A more recent study in Sweden by Hellgren et al evaluated the productivity loosed due to the common cold and allergic rhinitis and estimated the economic burden in Sweden alone was €2.7 billion annually. Of the total costs, absenteeism (44%) was the dominant factor, followed by presenteeism (37%) and caregiver absenteeism (19%) (2044).
There are no data on ARS, research is urgently needed.